Integration of family planning in nutrition programming: experiences from the Suaahara II programme in Nepal
This is a summary of a Field Exchange field article that was included in issue 64. The original article was authored by Basant Thapa, Manisha Laxmi Shrestha, Dr. Bhuwan Poudel, Ganga Khadka, Bijendra Banjade and Dr. Kenda Cunningham.
Basant Thapa is a family planning advisor for the Suaahara II programme.
Manisha Laxmi Shrestha is a nutrition specialist for the Suaahara II programme.
Dr. Bhuwan Poudel is Senior Public Health Administrator for the Bagmati Province Government in Health Office, Dhading, Nepal.
Ganga Khadka is a nutrition and health officer for the Suaahara II programme.
Bijendra Banjade is a nutrition and health officer for the Suaahara II programme.
Dr. Kenda Cunningham is the senior technical advisor for integrated nutrition and monitoring, evaluation and research for learning in the Suaahara II programme.
Background
In Nepal, approximately 17% of women of reproductive age (15-49 years) are thin. An equal proportion of adolescent girls (15-19 years) are pregnant with, or have had, their first child. Undernutrition and early pregnancy are associated with adverse nutrition and health outcomes, increasing the risk of low birth weight deliveries which continue the cycle of undernutrition into the next generation. While the prevalence of stunting (low height-for-age) among children under five years of age decreased from 57% to 36% between 1996 and 2016, wasting (low weight-for-height) prevalence in Nepal has persisted at around 10%.
Family planning (FP)1 and nutrition are intricately linked. Optimal birth spacing is associated with improved nutrition outcomes, while children from unintended pregnancies may be at risk of poor nutrition. Early pregnancy and childbearing can also have detrimental effects on the health, nutrition and development of adolescent mothers and their babies. While FP is often overlooked in nutrition programming, integration of these services provides opportunities for progress towards universal health coverage (as part of the 2030 Agenda for Sustainable Development) and improvements in health and nutrition outcomes for mothers and children. This should include harmonising FP counselling and services with maternal, infant and young child nutrition (MIYCN) services from pre-pregnancy to early childhood. This article explores an example of integration in Nepal, highlighting experiences and lessons learned.
Suaahara II programme
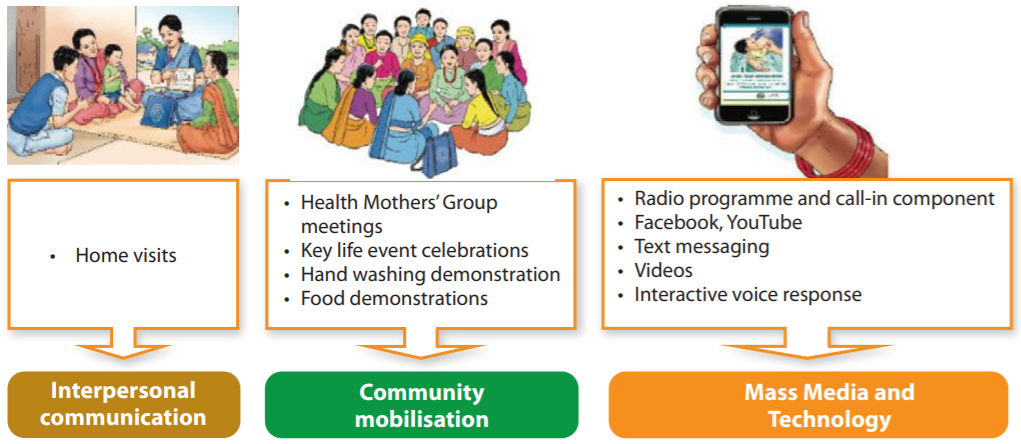
The Suaahara II programme (SII) is an integrated nutrition programme funded by the United States Agency for International Development (USAID) (April 2016 to March 2023) that covers 42 of Nepal’s 77 districts. Helen Keller International is the lead partner and the programme is implemented through a consortium with six other organisations, with another 39 partner non-governmental organisations implementing activities at district level. The aim of SII is to reduce undernutrition in Nepal, particularly among mothers and children within the first 1,000 days of life, through multi-sector interventions covering nutrition, health and FP, water, sanitation and hygiene, agriculture and markets and nutrition governance, using a gender equality and social inclusion approach. SII’s social and behaviour change strategies include inter-personal communication (primarily home visits by SII-hired frontline workers), community events, mass media (primarily a weekly radio programme also available on Facebook and YouTube) and text message communication (Figure 1). By September 2020, nearly two million households had been reached.
FP is integrated throughout SII household and community-level activities to improve knowledge and increase demand for high-quality FP services. For example, around 10% of the episodes of SII’s flagship weekly Banchhin Aama radio programme are dedicated to FP and the healthy timing and spacing of pregnancy (HTSP). Ideal FP is also promoted through social media platforms and a text message focusing on HTSP is sent to postnatal mothers. FP-related messages are integrated within the materials and job aids of SII’s frontline workers and the social and behaviour change communication (SBCC) materials used by female community health volunteers (FCHVs).
At the health service delivery level, the Government of Nepal’s (GoN) MIYCN training package for all health workers and FCHVs and related job aids have been revised to integrate FP and HTSP into nutrition services. As of September 2020, this training had been provided to all 2,111 health facilities in the 42 SII implementation districts.
Figure 1: Integrated SBCC approach of the Suaahara programme
Partnerships and linkages
SII works in partnership with the GoN to integrate FP and HTSP into various nutrition-related guidelines, protocols, training manuals and SBCC materials. SII actively participates in government-led Technical Working Group meetings, provides technical support and advocates for the scale-up of its integrated approach. SII community-based staff also collaborate with local government bodies around resource allocation and utilisation to address supply-side barriers. Additionally, SII collaborates with other development programmes to increase demand for integrated services and to promote best practices.
The integration of FP also goes beyond the health sector. For example, collaboration with the USAID-funded Knowledge-based Integrated Sustainable Agriculture project in Nepal included the integration of FP/HTSP messages into their training package which reached male farmers groups across 24 districts. FP and HTSP messages are also incorporated in the Health Mothers’ Group calendar used by FCHVs to facilitate systematic agenda-based discussions during monthly meetings.
Early indications of improvement
Findings from SII’s annual monitoring surveys suggest some modest but positive trends in FP indicators. For example, among a randomly selected sample of households with a child 0-5 years of age, the prevalence of women avoiding pregnancy increased from 40% to 44% between 2017 and 2019. The prevalence of married women using any modern method of FP also increased from 36% to 38% and the FP/HTSP knowledge among household heads (i.e., that a woman should wait to become pregnant until she is 20 years or older) increased from 52% to 53%. While promising, these results should be interpreted with caution in the absence of control groups and a more rigorous evaluation.
Implementation challenges
Government stakeholders at national and sub-national levels naturally have their own priorities and continuous advocacy for resource allocation has been required for successful integration. The limited time that health workers and FCHVs have for intervention activities has been a challenge and has meant that, at times, FP has been overlooked in favour of more urgent health and nutrition needs. Since quality assurance of integrated services and large-scale programmes can be challenging, SII has provided on-site coaching and mentoring to healthcare providers to ensure the delivery of high-quality services and build on knowledge and skills. Furthermore, the ability to reach disadvantaged populations with integrated services has also been a challenge since the barriers to behaviour change vary between populations. For example, communities struggling most to achieve dietary diversity may differ from those needing additional support to adopt modern FP practices. To mitigate the need for different targeting strategies by sector, SII regularly sharpens its targeting and behaviour change approaches.
Learnings and potentially replicable interventions
Integrated FP and nutrition programming provides opportunities to address knowledge gaps and generate demand for integrated services. Experience from the SII programme shows that using a range of communication channels to reach multiple household members ensures the consistent reinforcement of messages and promotes shared responsibility to increase the likelihood of desired behaviour changes. Continuous building of technical and management capacity, collaboration with a wide group of stakeholders and capacity building of facility- and community-based healthcare providers are central to effective implementation and scale-up. Working alongside government at all levels is also vital for long-term sustainability. In Nepal, a gradual increase in resources allocated through local level planning would help to sustain and improve the delivery of integrated services and contribute to providing a comprehensive package of essential health and nutrition services through universal healthcare coverage.
For more information, please contact Dr. Kenda Cunningham at kcunningham@hki.org
1 Family planning is defined by the World Health Organization as the ability of individuals and couples to anticipate and attain their desired number of children and the spacing and timing of their births.


