Transitioning nutrition programming from humanitarian aid to health system strengthening in Kenya
This is a summary of a Field Exchange field article that was included in issue 64. The original article was authored by Peter Hailey, Brenda Akwanyi, Emiliana Mbelenga and Tamsin Walters
Peter Hailey is the Director of the Centre for Humanitarian Change based in Nairobi.
Brenda Akwanyi is an independent consultant who has worked with Maximising the Quality of Scaling Up Nutrition Plus (MQSUN+)a since 2015.
Emiliana Mbelenga is a consultant with the Centre for Humanitarian Change.
Tamsin Walters is a partner at Nutrition Works who has worked with the MQSUN+ consortium.
Background
Maximising the Quality of Scaling Up Nutrition Plus (MQSUN+) provided technical support to the UK’s Foreign, Commonwealth and Development Office (FCDO) and UNICEF in Kenya between June 2018 and April 2020 to assess the implementation of the Kenya Nutrition Support Transition Programme and to examine the next steps once the programme had concluded. This article highlights some of the successes of the last 14 years and the remaining challenges in the transition towards government-led nutrition services.
Kenya’s arid and semi-arid lands (ASALs) experience recurring drought-related emergencies but responses have previously tended to be late and poorly coordinated. Associating nutrition programming with the drought response has also led to short-term and intermittent funding and programming. Since 2006, efforts have focused on establishing strong government-led nutrition services and nutrition partners have focused on health systems strengthening (HSS) activities.
A common vision for nutrition
After the 2006 emergency, a formal Memorandum of Understanding was established between UNICEF and partner non-governmental organisations (NGOs) to inform a common vision for nutrition. This was consolidated into a Partnership Framework involving the Ministry of Health (MoH), UNICEF, the World Food Programme and partner NGOs in 2009. The common vision included transitioning leadership and governance to the MoH and integrating nutrition services into existing health services. The government adopted the integrated management of acute malnutrition (IMAM) protocols in 2008-2009. By 2010, a package of 11 high-impact nutrition interventions had been embedded within the health system.
Continuous and inclusive coordination and communication
Nutrition coordination and communication was improved through the establishment of the MoH-led Nutrition Technical Forum and working groups (Figure 1). The Nutrition Interagency Coordinating Committeeb helped to ensure donor alignment with government priorities and now also constitutes the Scaling Up Nutrition multi-stakeholder platform. The Nutrition Response Advisory Group, now the Emergency Nutrition Advisory Committee, was also critical in guiding drought response at national and county levels.
Figure 1: Coordination for nutrition in Kenya showing technical working groups
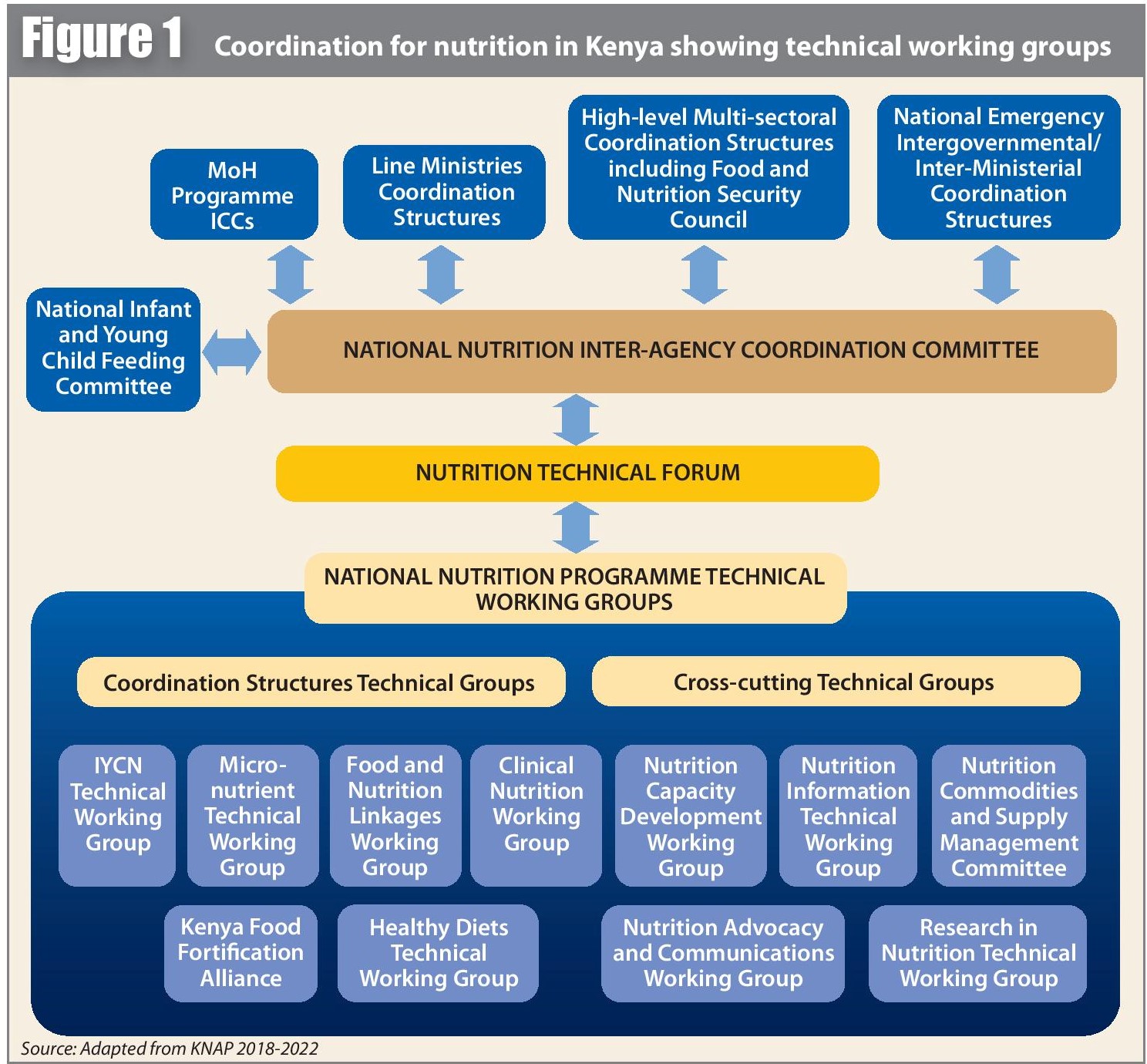
Source: Adapted from KNAP 2018-2022
Human resources for nutrition
There has been a progressive increase in the recruitment of nutritionists in most counties. Since 2010, donor-funded nutrition support officers (NSOs) have been embedded in national and county level MoH structures, providing technical assistance to the ASALs County Nutrition Coordinators. Evaluations in 2013 and 2017 noted the importance of NSOs at national and sub-national levels, however it is not yet clear how their roles can be sustainably transitioned to government positions.
Improved nutrition information systems
Nutrition information systems (NIS) have transitioned from primarily gathering and analysing information before and during emergencies to being used as a central health system tool. Parallel NGO and United Nations (UN) reporting systems and nutrition surveys were gradually integrated and, following a 2013 NIS evaluation, indicators and processes were standardised at the district/sub-county level and aligned to global standards. There was also investment in increased specialist NIS staff at UNICEF and at the MoH and training for health facility, sub-county and county staff on NIS activities. As a result, regular programme monitoring has seen significant improvements in the timeliness, completeness and quality of reporting. The focus is now shifting to strengthening the District Health Information System 2 with a nutrition lens.
Longer-term financing
Experiences during the 2011 drought highlighted the need for multi-year funding to ensure high-quality programming and services before, during and after a drought. Since 2012, donor funding for the UNICEF Maternal and Child Nutrition Programmes has gradually shifted towards development funds with supplementary emergency funds available during drought years. This longer-term view has enabled a focus on strengthening health system-related nutrition services.
The National Food and Nutrition Security Policy 2012-2017 and the National Nutrition Action Plan 2018-2022 have facilitated the mainstreaming of nutrition budgeting into national and county-level development plans. The National Drought Management Authority introduced a government-managed Drought Contingency Fund in 2014 from which, by 2016, health and nutrition services benefited. In 2019, National Government Emergency Response Funds were allocated to nutrition services and County Contingency Funds have been part of the response.
Supply chain strengthening
Since 2011, IMAM supplies have been included in the essential medicines list. Supply chain quality and management was included in the 2012-2017 National Nutrition Action Plan and the scale-up of the logistics management information system since 2017 has led to measurable improvements in supply chain management and reporting. The MoH, UNICEF and the Kenya Medical Supplies Authority jointly monitor progress. However, sustainable financing for ready-to-use therapeutic food requires urgent attention as it remains highly dependent on donor funding.
Innovations in nutrition health systems
The community-based management of acute malnutrition (CMAM)/IMAM surge approach, developed by Concern Worldwide and partners, has been a valuable tool in drought-prone areas in the country, helping to build a resilient health system. Adoption and rollout of the approach in the ASALs contributed to the timeliness of the 2019 drought response.
Two innovations have considerably increased the effectiveness and coverage of outreach services in the sparsely populated ASALs. Firstly, the integration of a basic package of health and nutrition services has reduced duplication of outreach services. Secondly, the use of county outreach deployment plans since 2016 has aided the prioritisation of malnutrition hotspots and informed scale-up. However, the current use of externally funded mechanisms to achieve universal health coverage is unsustainable. Incorporating alternative approaches such as integrated Community Case Management (iCCM)-IMAM and task shifting to community level are important next steps.
Community capacity for nutrition services and indications of progress
Since the rollout of the Community Health Strategy (CHS) in 2006, civil society actors and faith-based organisations (FBOs) have complemented government efforts through community units which empower communities to manage their own health. Partners (UNICEF, NGOs and FBOs) have assisted in capacity building of community health extension workers (employed by the MoH) and community health volunteers (CHVs) to deliver nutrition services.
By 2017, there were noted improvements in the early detection, identification and referral of acute malnutrition cases. This contributed to increased admissions for severely wasted children from 21,658 in 2009 to 87,622 in 2019. Despite higher admissions, recovery rates remained relatively unchanged. The new Community Health Policy 2020-2030 aims to streamline the implementation of the CHS. However, questions around sustainability, including incentivising CHVs, remain.
Moving forward and building on successes
Over the last 14 years, nutrition programming in Kenya has shifted from a parallel UN and NGO ‘emergency’ approach to a government-led and managed nutrition service within the health system. Progress has been made towards achieving the common vision for nutrition and an HSS approach has been used to support the government to provide high-quality health and nutrition services. This process has benefited both ‘regular’ nutrition services and the nutrition drought response. However, a faster transition from a donor- to government-financed system is needed and nutrition must be further embedded into the health system financing strategy.
A common vision and coordination structure, as well as UNICEF and donor support, have been fundamental to progress. Priorities for the next five years include refreshing the common vision for health system-based nutrition services and transitioning further away from aid.
For more information, please contact Peter Hailey at peter.hailey@whatworks.co.ke
a MQSUN+ provides the FCDO and the Scaling Up Nutrition (SUN) Movement with technical services to improve the quality of nutrition-specific and nutrition-sensitive programmes. The project is resourced by a consortium of five leading non-state organisations which is led by PATH.
b The NICC has representation from various agency heads and government line ministries.


