Costing delivery of severe wasting treatment in Indonesia
This is a summary of a Field Exchange field article that was included in issue 69. The original article was authored by Lani Trenouth, Blandina Rosalina Bait, Markus Harmiko, Julia Suryantan, Sidayu Ariteja, Nida Rohmawati and Ruth Laiskodat.
Lani Trenouth is a former consultant with the UNICEF Regional Office for South Asia.
Blandina Rosalina Bait is a Nutrition Specialist with UNICEF Indonesia.
Markus Harmiko is a former Nutrition Officer with UNICEF Indonesia.
Julia Suryantan is a Nutrition Officer with UNICEF Indonesia.
Sidayu Ariteja is a Planner at the Ministry of National Development Planning, Indonesia.
Nida Rohmawati is the Chief Coordinator of the Task Force for Under Five and Preschool Children at the Ministry of Health, Indonesia.
Ruth Laiskodat is the Head of the Provincial Health Office, East Nusa Tenggara, Indonesia.
Key messages:
- A costing exercise estimated that an annual investment of USD 4.8 million was required to achieve the Government of Indonesia’s 2024 target of 90% treatment coverage in 60% of all primary healthcare centres in East Nusa Tenggara (NTT) province, Indonesia.
- The findings also indicated that scale-up efforts should prioritise improving treatment coverage to achieve better cost-efficiency of integrated management of acute malnutrition (IMAM) services in high-burden areas.
Background
In Indonesia, the 2021 Presidential Decree on child stunting set the ambitious target of providing treatment to 90% of severely wasted children by 2024. To achieve this, the Ministry of Health (MoH) plans to ensure that at least 60% of all primary healthcare centres (puskesmas) provide integrated management of acute malnutrition (IMAM) services by 2024. Although IMAM services are provided in all provinces of Indonesia, scale-up is restricted by a lack of evidence on cost, cost-efficiency and cost-effectiveness.
In 2021, the United Nations Children’s Fund (UNICEF) conducted a costing exercise using IMAM data collected from Kupang Municipality and Kupang District in East Nusa Tenggara (NTT) province. The goal was to estimate the cost and cost-efficiency1 of the IMAM programme (measured as the cost per child admitted for treatment of severe wasting) and to estimate the financial resources required to achieve the government’s coverage target.
Approach
Data on resource usage for the IMAM programme were collected from Kupang District and Kupang Municipality. This included data on all costs carried by implementing institutions, including for community mobilisation, outpatient treatment for uncomplicated cases, inpatient treatment for complicated cases and infants below six months of age, and overall programme management and oversight.
The analysis involved the following steps: (1) identification of the resources used to implement the IMAM programme; (2) estimation of the required number or volume of each resource; (3) determination of the unit cost of each resource; and (4) multiplication of the total volume of resources required by the unit cost of each resource to estimate the total cost of the IMAM programme at a given scale. For example, the total cost of treatment (personnel time per child) was calculated by multiplying the average time spent with a child at the outpatient care site by the cost of personnel time, based on standard salary grids provided by MoH.
Findings
Programme performance
- 297 children were admitted for wasting treatment in Kupang District and Kupang Municipality. Of these, 72 were initially admitted to inpatient care before being discharged to outpatient care.
- Inpatient care lasted an average of seven days for children aged 6-59 months and an average of 21 days for children aged below six months. Outpatient care lasted an average of six weeks.
- Outcome data were unavailable, so it was assumed that all children admitted were discharged to outpatient facilities, and that no defaulting occurred during outpatient care.2
- On average, 14.6 kg of ready-to-use therapeutic food (RUTF) was used per child in outpatient care.
- Each child admitted to outpatient care received, on average, 1.1 days of aggregate staff time over six weeks of treatment, or 1.5 hours per visit. For inpatient care, each child received 1.9 days of aggregate staff time over seven to 21 days, or 1.2 hours per day.
Cost-efficiency
- The total cost of providing IMAM services for one year was estimated at USD 96.725.
- Cost-efficiency (total cost divided by the number of children admitted for treatment (N = 297)) was estimated as USD 326 per child admitted for severe wasting treatment.
Cost drivers
- The largest drivers of the cost of the IMAM programme were personnel costs for community outreach and screening (28%), followed by RUTF costs (13%) and supply logistics for RUTF transportation and storage (8%).
Cost modelling
Cost projections were conducted by identifying the cost categories that vary with the caseload (such as RUTF or treatment staff time) and those that vary with the number of care sites (such as non-consumable clinic supplies or middle management supervision time).
To estimate changes in costs relative to the scale-up of treatment services, treatment coverage and geographic coverage scenarios were modelled.
- Treatment coverage was calculated based on the total number of children admitted for treatment of severe wasting at the care sites in Kupang District and Kupang Municipality (N = 297), and as a percentage of the estimated district burden using reported prevalence of severe wasting in children under five years of age during the reference period (N = 9,357).
- Geographic coverage of the IMAM programme was estimated at 13%, based on the number of posyandu3 providing IMAM services (N = 647), divided by the total number of posyandu (N = 5,136).4
- The modelled coverage percentages were based on MoH’s progressive targets for IMAM services up to 2024. At the time of analysis, the estimated IMAM treatment coverage was 3.2%.
- The annual cost of achieving the government’s 2024 target of 90% treatment coverage in 60% of all puskesmas in NTT province was estimated at USD 4.8 million (Table 1). To achieve a global average treatment coverage of 40% and geographic coverage of 43%, an estimated USD 1.8 million would be required.
- The costing projections highlight that greater cost-efficiency could be achieved through improving treatment coverage within selected high-burden districts than could be achieved by increasing geographic coverage without improving treatment coverage.
Table 1: Cost and cost-efficiency projections based on treatment coverage and geographic coverage for NTT province*
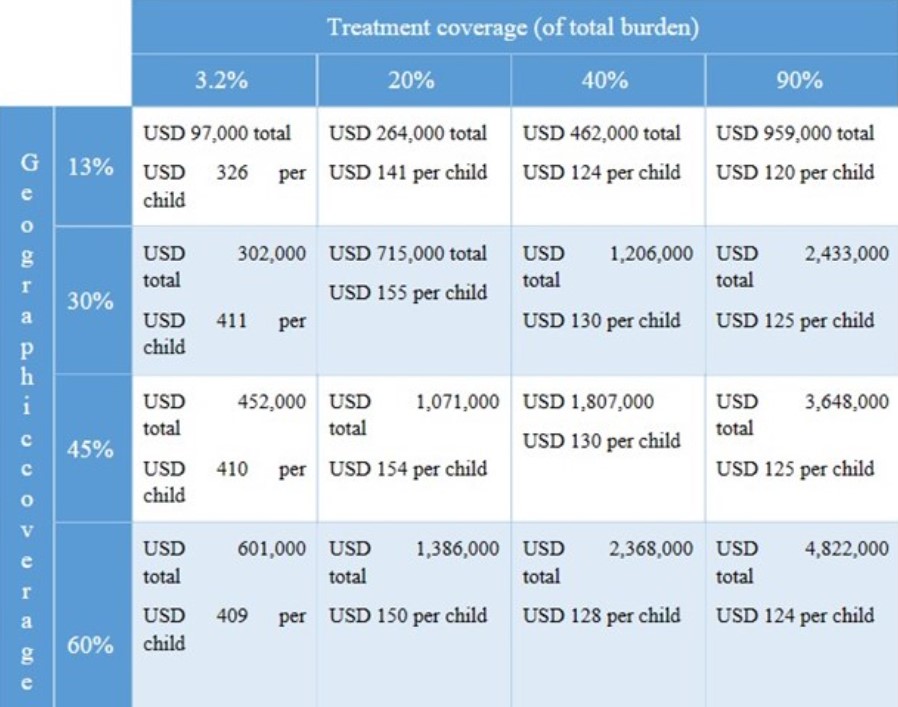
* Cost estimates are rounded to the nearest USD 1,000.
Conclusions
This exercise provided valuable insight into the financial resources required to scale up IMAM services and achieve the Government of Indonesia’s targets by 2024. However, given contextual and epidemiological variations in severe wasting across Indonesia, additional costing exercises in other provinces are needed to better estimate national-level investment requirements. In 2022, the total budget allocation for nutrition services, including treatment and prevention of child wasting, was USD 2.95 billion. Approximately 3% of children affected by severe wasting in Indonesia live in NTT. For the province to achieve 90% treatment coverage, approximately 0.16% of the national budget for nutrition interventions would be required.
The findings from this exercise show that the cost-efficiency of IMAM services increases as treatment coverage improves. This suggests that scale-up efforts should prioritise increasing treatment coverage in high-burden areas.
For more information, please contact Blandina Rosalina Bait at bbait@unicef.org.


