Lessons learned from the 2011/2012 Kenya blanket supplementary feeding programme
by Joyce Owigar Joyce is currently the Programme Officer for Nutrition within the World Food Programme in Kenya, where she has been working since 2007.
Due to recurring drought in the arid counties of Kenya, WFP and the Nutrition Sector in Kenya have implemented Blanket Supplementary Feeding Programmes (BSFPs) to prevent nutritional deterioration in vulnerable groups (particularly children less than five years of age, and pregnant and lactating women). In July 2011, in response to high levels of Global Acute Malnutrition (GAM) due to the failure of the short and long rainy seasons, BSFPs were implemented in six arid counties: Turkana, Mandera, Wajir, Isiolo, Samburu and Marsabit.
The BSFP provided a package of essential health and nutrition services including screening for acute malnutrition, health and nutrition counseling and systematic treatment, alongside food distributions (consisting of fortified corn soy blend and vegetable oil).
From the start of the BSFP, the nutrition situation was monitored through nutrition surveys and by screening all clients at each distribution. Nutrition surveys in June through November documented decreasing GAM levels.
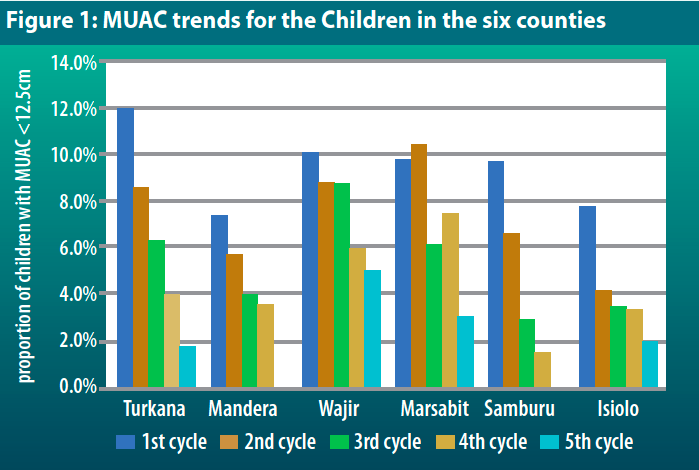
Anthropometric screening (MUAC and oedema) throughout the course of the intervention demonstrates an improving nutritional status among children less than five years in successive distributions.
The overall decrease in GAM prevalence and MUAC trends for children were a positive step but it is recognized that other factors and/or programmes could have also contributed to the improved nutrition situation (Figure 1).
Achievements
Quick start. A key achievement of the BSFP was the ability to start implementation in a relatively short period of time. The 2011/2012 BSFP started in the most severely affected region, Turkana North, within one month of the release of nutrition survey findings indicating 37% GAM. The intervention started within the second month for the other critical counties, prioritizing children less than three years of age and pregnant and lactating women for the first and second distributions and including all children less than five years of age from the third distributions. The development of a BSFP implementation strategy and good coordination among implementing partners greatly facilitated the process.
Good coverage. Planned coverage was surpassed due to extensive community mobilization activities and quality rations provided. The following table shows the planned coverage compared to actuals during the BSFP (Table 1).
| Table 1 | |||||||
| Districts |
CYCLE Beneficiaries |
||||||
| Planned | Cycle 1 | Cycle 2 | Planned | Cycle 3 | Cycle 4 | Cycle 52 | |
| ISIOLO | 33,358 | 13,629 | 15,751 | 37,289 | 25,562 | 27,266 | 33,968 |
| MANDERA | 103,292 | 93,138 | 118,090 | 146,826 | 166,170 | 179,142 | - |
| MARSABIT | 27,503 | 28,049 | 30,501 | 46,577 | 45,233 | 46,488 | 46,581 |
| SAMBURU | 30,016 | 35,026 | 46,996 | 59,609 | 58,210 | 60,774 | - |
| TURKANA | 81,805 | 73,270 | 92,189 | 139,933 | 135,288 | 131,682 | 125,774 |
| WAJIR | 86,297 | 86,763 | 98,505 | 193,661 | 185,173 | 196,165 | 200,845 |
| Grand Total | 362,271 | 329,875 | 402,032 | 623,895 | 615,636 | 641,517 | 407,168 |
| Proportion of Target |
100% | 91% | 111% | 100% | 99% | 103% | 98% |
Lessons learned
Several lessons were learned from the implementation of the 2011-2012 BSFP.
Comprehensive package of interventions: Children and women who had not received immunizations and supplementation1 received these services during the BSFP. Beneficiaries also received health education and were referred for medical services where necessary. However, while food was readily available during the first and second cycles, immunizations and supplements were only available from the third cycle.
Lesson: Comprehensive planning and coordination from the onset by the nutrition sector and others, including the Division of Immunization within the Ministry of Health, would ensure a more harmonized approach.
Stock Prepositioning: Sourcing sufficient commodities (CSB and oil) quickly was a challenge. Insufficient stocks in the beginning prevented targeting of all children under five years. Priority was given to children less than three years, and pregnant and lactating women for the first two distributions.
Lesson: There is need to ensure an immediately available stock of nutrition supplies for emergency response. In 2011 WFP established a Forward Purchasing Facility at the East Africa regional level that aims to ensure stock contingencies are available to countries for specific regions. As a result, countries are better prepared for emergencies in terms of availability of supplies.
Response Planning: The BSFP was planned for five distributions during five months (August – December 2011) with the expectation that the food security and nutrition situation would have improved by early 2012 due to the October – December 2011 rainy season. However, due to delays in food supplies and washed out roads, the BSFP continued until March 2012 (eight distributions). This resulted in additional challenges as some of the operational costs such as some level of staffing, office premises and vehicles were maintained throughout the extended implementation period. Additionally, food insecurity and vulnerability to undernutrition was different across the counties and some needed longer support while others did not.
Lesson: The timing and type of response should be designed based on the context of each area.
Early Warning Information: The existing nutritional surveillance data (based on MUAC screening) available in late 2010 and early 2011 was not credible and thus nutrition surveys were conducted. Surveys were carried out during the peak of the dry season and reflect the situation during the worst period. The BSFP was implemented to prevent a further deterioration in the malnutrition levels, but ideally should have been implemented much earlier.
Lesson: Existing surveillance systems should be supported to indicate a deteriorating situation to allow for a response to mitigate an emergency. Alternatively, surveys should be carried out earlier to allow for a timely response.
BSFP and IMAM linkage: In the BSFP strategy, individuals identified with acute malnutrition were to be referred to the Government of Kenya’s Integrated Management of Acute Malnutrition (IMAM) programme. However, practically linking individuals proved to be challenging in areas where there was limited capacity for IMAM.
Lesson: For future programming, BSFP implementation should be planned alongside existing IMAM interventions to ensure full integration. Additional inputs (staff, vehicles and supplies) for IMAM implementation may be required to ensure effective linkage.
Human Resources:
Staffing: Learning from the 2010 BSFP in Kenya, the 2011/2012 BSFP developed and implemented an elaborate staffing strategy with a total of 21 staff for every 250 beneficiaries for a given site as shown in box 1.
Box 1: Composition of a distribution team for every 250 beneficiaries:
- 4 screeners (Oedema, Height and MUAC)
- 2 registrars
- 5 crowd controllers
- 4 distribution staff (2 CSB and 2 vegetable oil)
- 2 loaders (CSB and Vegetable oil replenishment)
- 1 verification staff (ink printing)
- 1 CHW (Nurse assistant)
- 1 Nurse (distribution of systematic treatment and immunizations)
- 1 Supervisor
Due to the urgency of the interventions, not all the required staff could be recruited on time, and therefore recruitment continued during the course of implementation.
Trainings: The quality of trainings varied. Trainings conducted at the onset of the response were longer and provided more detail than later trainings.
Staff turnover was high and therefore, there was a continual need for training. Recruitment of skilled staff, in particular nurses, within a very short period of time was also a challenge. Nurses were not readily available in the counties, and a number of partners had to source from neighboring counties or contact medical training colleges. This contributed to the delays in implementation of the systematic treatment component of the programme.
Lessons: Training should be a constant feature, with allocated funding for routine training. To reduce the high staff turnover, BSFP staff should have flexible contracts for the duration of implementation as opposed to casual contracts (which will in turn reduce the amount of trainings required). For skilled staff such as nurses, a pool of nurses should be identified for emergency recall by the health sector, to ensure availability on short notice to effectively respond to future emergencies.
Documentation: The 2011/2012 BSFP developed an elaborate reporting system in which routine process monitoring data (number of beneficiaries, screenings, systematic treatment and stock reports) was collected from each distribution site by implementing partners and submitted to Save the Children (SCUK), who was the lead process monitoring partner. SCUK consolidated these reports and generated monthly/cycle BSFP progress reports which were the basis for discussion and follow up actions at national and county levels. Hellen Keller International also monitored the qualitative aspects of the programme and generated monthly/cycle reports also for discussion and follow up. These reports were supposed to feed into routine government reporting; however, the majority did not because reports either did not reach health facilities or did reach but were not consolidated with routine reporting at facility level. As a result, the number of beneficiaries that received systematic treatment through the BSFP was not reported in County health facility reports.
Lesson: BSFP data collection and reporting should be integrated into routine health management information systems and the documentation process, formats and requirements should be clear to all stakeholders from the start.
1For children- Vitamin A and zinc for diarrhea treatment. For pregnant women – iron/folate, deworming and tetanus toxoid vaccine. For lactating women – vitamin A.
2The fifth cycle was not planned for Mandera and Samburu, given the change in seasons and reduced vulnerability

