Tackling high defaulting rates in refugee camp settings – lessons from Chad
 Seife Kifleyohannes Temere
Seife Kifleyohannes Temere
Seife Kifleyohannes Temere is a Nurse Nutritionist. He has been working for International Medical Corps since 2010.
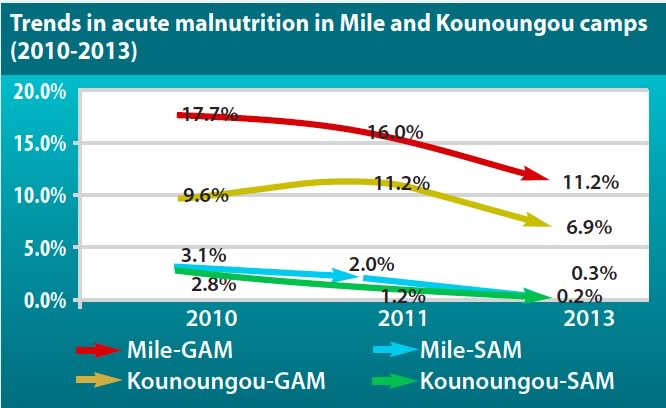
In eastern Chad there are 12 Sudanese refugee camps. Since 2004, IMC has been providing nutritional support in two of these camps: Mile and Kounoungou. The nutrition situation is precarious with a high prevalence of acute malnutrition. The Global Acute Malnutrition (GAM) has surpassed the WHO ‘emergency’ thresholds in the past, though in 2013 the GAM rate declined in all camps compared to 2010 and 2011 (see graph below). Micronutrient deficiencies are also prevalent; a UNHCR/IMC survey in January 2013 documented a prevalence of anaemia in 6-59 month olds at 52.6% (Mile) and 46.8% (Kounoungou). The refugees in these camps are highly dependent on humanitarian assistance and food aid.
Programme review
 During 2010 and 2011, IMC’s nutrition support mainly focused on the treatment of SAM and MAM; however, neither IMC nor other partners were involved in prevention activities or studies to understand the underlying causes of acute malnutrition in the camps.
During 2010 and 2011, IMC’s nutrition support mainly focused on the treatment of SAM and MAM; however, neither IMC nor other partners were involved in prevention activities or studies to understand the underlying causes of acute malnutrition in the camps.
In 2012 UNHCR, in collaboration with IMC, conducted a causal analysis of acute malnutrition in Mile camp. The causal framework of malnutrition (ACF/UNICEF) was used in addition to select socio-anthropological and health tools to identify the underlying causes of malnutrition. A literature review was conducted, assumptions around underlying causes were identified and discussed in workshops, and information was collected from individuals, focus groups and through observation to triangulate findings. The underlying causes of undernutrition in the camps were identified as a 1) shortage of food (food aid does not cover the refugee’s household food needs for a full month and refugees were selling part of this ration to increase their purchasing power); 2) lack of access to clean drinking water; and 3) lack of knowledge on infant and young child feeding practices.
Routine programme data were reviewed to further understand the situation. Data for the month of January showed persistently high default rates in the targeted Supplementary Feeding Programme (TSFP) and outpatient therapeutic care programme (OTP) as shown in the table 1.
| Table 1 | ||
|
Camp |
% Defaulters (Jan 2012) | |
| TSFP | OTP | |
| Mile | 24.2% (16) | 16.7% (3) |
| Kounoungou | 19.2% (10) | 17.4% (4) |
The defaulter rate was well above the Sphere minimum standard of < 15%. High defaulter rates translate into poor programme coverage as children leave the programme before they have recovered. Non-response may also be linked to default because mothers may decide to discontinue their child’s participation in the programme if they don’t see significant improvement in their child’s well-being.
To investigate why there was such a high defaulter rate, a defaulter study was conducted. The study documented a number of barriers to bringing children to the programme. The most important barriers identified were the need for frequent travel outside the camp to visit family members (in other camps or in Sudan), collecting firewood, and daily waged labour. Other barriers and challenges to attendance included:
- When the child was sick, traditional beliefs suggested that a traditional healer could cure the illness. Mothers would therefore visit a traditional healer first, often bringing a child to the OTP or TSP for nutrition treatment after they had exhausted traditional healing options.
- The small ration given (2.8 kg every 2 weeks) was reportedly not worth the effort to enrol in the programme and culturally, the small ration was shared between all the children.
- The quality of CSB was sometimes poor due to poor storage conditions.
- The CSB was perceived to cause diarrhoea.
- There was over-crowding in the health centers.
- The former blanket supplementary feeding programme had become targeted, thus putting people off from attending particularly pregnant and lactating mothers.
Revised programme activities
Following the results from the defaulter assessment, and with the support of UNHCR, the IMC nutrition team focused on the following key activities to reduce the high defaulter and malnutrition rates.
- Training was conducted for the traditional healers in the identification and referral of children and pregnant and lactating women to the programme. Many traditional healers became de-facto volunteers of the programme, assessing children using Mid-Upper-Arm-Circumference (MUAC) and referring low MUAC children to the programme.
- During discussions with mothers/carers (at health centres) and the whole family (during home visits) emphasis was placed on PlumpyNut and CSB as being a treatment and not just a food.
- Integrating the provision of health and nutrition assessment and care. The provision of PlumpyNut was provided by health staff during antenatal and prenatal visits at health clinics or through home visits by traditional birth assistants or community health workers.
- Widened screening criteria. Chadian nutrition protocols use both MUAC and WFH for admission. To ensure that MUAC screening identified all low WFH children, a MUAC off < 140 mm was used to initially screen children1.
- Conducting community sensitisation during the general food distribution as, while families travel significantly, they usually return for the GFD distribution (at the beginning of the month).
Results
After implementing these activities, the annual default rate decreased as shown in the table 2.
| Table 2 | ||||||
|
|
T-SFP Overall defaulter rate per year |
OTP overall defaulter rate per year |
||||
| Camp | 2011 | 2012 | 2013 | 2011 | 2012 | 2013 |
| Mile | 16.3% | 12.2% | 6.1% | 13.1% | 10.7% | 4.8% |
| Kounoungou | 16.8% | 9.5% | 4.7% | 17.3% | 11.2% | 7.0% |
Conclusion
Through a comprehensive review of the programme and investigation into the causes of defaulting, UNHCR and IMC identified the key barriers to achieving better programme coverage and impact. Concrete steps to address these barriers have been taken and the default rate has improved. However, the nutrition situation remains precarious and IMC recognises that there is still much to do to prevent and treat undernutrition in the camps. In May 2012, IMC in collaboration with UNHCR began distributing Nutributter®, a lipid-based nutrient supplement, to children 6-24 months old to prevent acute malnutrition. In addition, IMC plans to continue defaulter tracing and start new activities to further improve infant and young child feeding practices and micronutrient deficiencies.
For further information, please contact Seife Kifleyohannes Temere by email stemere@internationalmedicalcorps.org
1Children not eligible for the programme are congratulated and the carer is provided with a bar of soap.

