Providing maternal nutrition services at sub-national level in Punjab Province, Pakistan
Dr Khawaja Masuood Ahmed is the National Coordinator for Nutrition and for the National Fortification Alliance in the Ministry of Health, Pakistan.
Dr Saba Shuja is a medical doctor and Nutrition Officer with UNICEF, Pakistan.
Dr Wisal Khan is a medical doctor and Nutrition Specialist with UNICEF, Pakistan.
Introduction
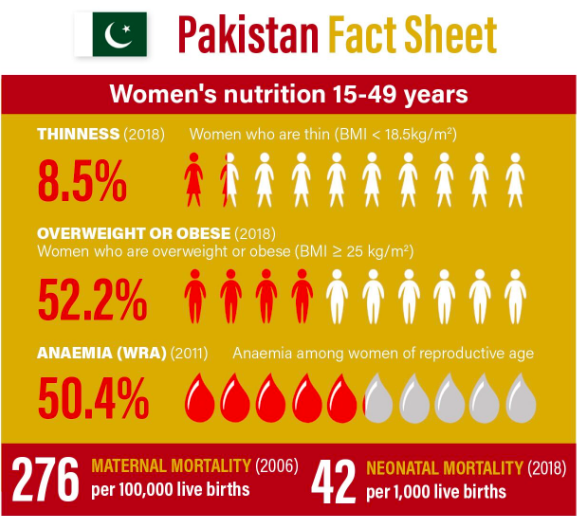
Pakistan is the sixth-largest country in the world, with a population of more than 200 million, and projected to be the fourth-largest by 20501. The nutritional status of the population is generally poor throughout the country, especially among children under five years old, women of reproductive age and the elderly. About 9% of adult Pakistani women are thin or undernourished (BMI <18.5 kg/m2), while overweight or obesity among women has increased from 40% in 2012-13 to 52% in 2017-182. Micronutrient deficiencies are also endemic among Pakistani women and almost 50% of women in Pakistan suffer from anaemia3.
The country has a decentralised government administration, with programme implementation and spending on health services devolved to provincial level. This article describes how maternal nutrition policy and programme action have been enabled within this devolution framework in the country’s largest province, Punjab.
National-level policy and antenatal care
The Government of Pakistan is committed to improving health outcomes in reproductive, maternal, new-born and child health across the country. While the national health policy has clear provisions for addressing maternal health, it lacks comprehensive provisions for addressing maternal nutrition, apart from micronutrient supplementation during pregnancy and lactation.
The lack of a robust and coherent policy response to maternal nutrition challenges in the country translates to significant gaps in the public service delivery of recommended, evidence-based maternal nutrition interventions and sub-optimal coverage. To address these gaps, Pakistan is in the process of developing a national adolescent and maternal nutrition strategy, which is expected to be released by the end of 2019. This will be followed by the development of provincial action plans.
Delivering maternal services
Notwithstanding these policy constraints, opportunities offered by decentralisation have led to improvements in service delivery at the sub-national level. The Government of Pakistan has mandated the provision of free antenatal care (ANC) services, including iron folic acid (IFA) supplementation. These services are available at both government-run health facilities and at community level, where they are delivered by lady health workers (LHW), Pakistan’s cadre of salaried community health workers. Despite availability of these services, low consumption of IFA supplements (44%) persists throughout the country3.
According to the most recent Pakistan Demographic Health Survey (DHS) (2017-2018), there have been some improvements in the utilisation of maternal health services. In the last five years, provision of ANC by skilled healthcare providers increased from 73% to 86%, while attended births at health facilities increased from 48% to 66%2. This is yet to translate into improvements in maternal nutrition coverage indicators, however, and tracking of progress remains impeded by measurement gaps in national data systems. For example, maternal nutrition micronutrient deficiency-related indicators at provincial level, such as anaemia, have yet to be measured under the forthcoming National Nutrition Survey (NNS 2018-2019), since this type of biochemical data is not collected in the Pakistan DHS.
Developing an integrated programme at sub-national level
The decentralised context of public service delivery in Pakistan has led to some positive improvements in the health planning processes and prioritisation of the delivery of integrated programmes. In Punjab, the provincial administration recognised the similarity and frequent overlap in the service delivery mechanism across different programmes and programme components, such as the maternal, newborn and child health; nutrition; reproductive health; and LHW programmes.
In 2013 the Government of Punjab took the decision to bring these four programmes under the same umbrella to ensure greater coordination and collaboration, thus creating the province’s Integrated Reproductive, Maternal, Neonatal, Child Health and Nutrition (IRMNCH&N) programme. Maternal nutrition is one of the 10 components of the IRMNCH&N and aims to develop and implement preventive and curative nutrition services for mothers and children through its nutrition service delivery model.
To operationalise the programme, a provincial IRMNCH&N action plan for Punjab province has been developed in line with the priority areas envisaged in the Ten Point National Vision on RMNCAH & Nutrition formulated by the Ministry of National Health Services Regulations & Coordination. Its alignment with the Punjab Health Sector Strategy (2012-2020) has also been ensured, with one of the key objectives in the strategy being to institutionalise the quality of care in the nutrition services delivery system.
Strengthening support for maternal health and nutrition
The IRMNCH&N is a vertical programme that uses existing governance and implementation structures at province level to deliver maternal nutrition interventions. Currently, the IRMNCH&N is implemented throughout Punjab with a workforce of over 55,000 health workers. The programme for family planning and primary healthcare (the LHW programme) has 44,500 LHWs and 1,800 lady health supervisors (LHS), with an additional 3,000 community midwives trained through the maternal and neonatal child health programme. LHWs are based in the community and conduct home visits for health promotion and supplementation activities (mainly IFA), acting as a bridge between community-based and facility-based services.
The IRMNCH&N programme has been further strengthened through ongoing 24/7 primary healthcare with the support of 4,000 lady health visitors (LHVs) for maternal health and nutrition care. LHVs are stationed mainly at health facilities and assist medical doctors in performing maternal and child health-related duties.
The initiative to address maternal nutrition at sub-national level has a unique approach under the IRMNCH&N programme as it has engaged different ongoing programmes (as described above) in a single platform to ‘deliver as one’. The health workforce at facility level, such as LHVs responsible for maternal health, has a strong referral link with the community workforce (i.e., LHWs and community midwives).

Improving outcomes for women
These efforts have brought considerable improvements in maternal health and nutrition status in Punjab. Out of Pakistan’s six provinces, Punjab has the highest percentage of women receiving antenatal care from a skilled provider (92.3% in 2017-18). The proportion of deliveries assisted by a skilled birth attendant increased from 52.5% in 2012-13 to 71.3% in 2017-18 and the proportion of facility deliveries also saw a considerable rise (from 48.5% in 2012-13 to 69% in 2017-18)4.
Moreover, through the integrated service delivery model, approximately 1.9 million pregnant and lactating women are being screened by LHWs in covered areas and around 17,701 are referred for the treatment of maternal undernutrition annually. About 0.3 million pregnant women were provided with IFA tablets and approximately 1.1 million pregnant and lactating women were counselled on dietary diversity5.
Training frontline workers
Capacity-building initiatives for community and facility-based health workers on maternal nutrition has improved the coverage of maternal nutrition interventions. To date in the province, 600 healthcare workers have been trained as master trainers and 43,000 LHW/LHS have been trained using a Punjab-specific nutrition manual (developed in 2018), which includes maternal nutrition as an integral part of the curriculum.
Challenges with multi-sector coordination
The IRMNCH&N programme has a number of potential options for building linkages with other sectors to address underlying causes of maternal malnutrition, via both the multi-sector nutrition centre (MSNC) led by the Planning and Development Department, and through the Policy and Strategic Planning Unit within the Punjab Health Department. However, despite these existing mechanisms for inter-sector coordination and planning, the role of various line departments, such as education, agriculture, labour and industry and water and sanitation, in contributing towards the health and nutrition outcomes of women is almost negligible. Multi-sector engagement for maternal nutrition service delivery is still not well connected and requires greater effort in the province.
Next steps
The Government of Punjab has launched several new initiatives to improve maternal nutrition, the most important one being the integration of a number of overlapping programmes and initiatives under one umbrella. The key lesson learned in Punjab province is that maternal nutrition services are best delivered through the primary healthcare system with the involvement of community health workers. Next steps are to finalise the sub-national development of health services packages for secondary and tertiary care level.
An integrated Punjab Health Information System has been developed for effective monitoring and evaluation and is being rolled out. Finally, maternal nutrition will be further strengthened with the adoption of the national adolescent and maternal nutrition strategy, currently being formulated. This strategy will be used to inform existing and future planning of maternal nutrition interventions in the province.
Footnotes
1Pakistan Bureau of Statistics http://www.pbs.gov.pk/content/population-census
2Pakistan Demographic and Health Survey (2017-2018)https://dhsprogram.com/pubs/pdf/SR257/SR257.pdf
32016 https://data.worldbank.org/indicator/SH.ANM.ALLW.ZS
4Multiple Indicator Cluster Survey, Punjab (2017-2018) and Punjab Health Survey.
5IRMNCH&N programme data (2018).

