In Chad, the Mother-MUAC approach improves treatment access for malnourished children
In Chad, the Mother-MUAC approach improves treatment access for malnourished children
By Hyppolite Gnamien, Chantal Autotte Bouchard, Jean-Robert Bwanaissa Shabani, Emily Helary and Marion Blanloeuil
Hyppolite Gnamien is a medical doctor specialising in public health. Hyppolite is the Medical Coordinator of the Première Urgence Internationale mission in Chad.
Chantal Autotte Bouchard is a nurse specialising in malnutrition, public health and tropical medicine. Chantal is the health and nutrition referent for Première Urgence Internationale Headquarters.
Jean Robert Bwanaissa Shabani is a medical doctor specialising in public health. He is the Health/Nutrition Technical Manager in Ouaddaï for the Première Urgence Internationale mission in Chad.
Emily Helary is a Program Officer at Première Urgence Internationale Headquarters.
Marion Blanloeuil is Desk Assistant at Première Urgence Internationale Headquarters.
The activities described in this article are implemented by Première Urgence Internationale in partnership with the Provincial Health Delegation of Ouaddaï, Chad, thanks to the support of UNICEF and the European Union through the Directorate-General for European Civil Protection and Humanitarian Aid Operations (DG ECHO).
Location: Chad
What we know: Screening for malnutrition is increasingly conducted by family members as a means of enabling broader and earlier detection of child malnutrition.
What this article adds: In 2018, the non-governmental organisation, Première Urgence Internationale, introduced the ‘Mother-MUAC approach’ into its nutrition programme in the Ouaddaï province of Chad. Screening coverage increased from 79.6% when using the previous approach (screening conducted by community health workers (CHWs)) to 85.5% (screening conducted by family members). An increased percentage of children diagnosed with severe wasting were also admitted for treatment at a health facility (63.2% in the Mother-MUAC approach versus 50.2% in the CHW approach). Therapeutic treatment performance indicators were comparable between both strategies. Results also demonstrated strong acceptance by mothers of the Mother-MUAC approach, both by mothers doing the screening and by mothers whose children were screened by mother-peers. Health staff are also highly supportive of the approach due to the improved programme coverage and the cooperation of caregivers. In addition, the programme support costs were reduced by 27% according to average support cost per health centre. In this programme, the Mother-MUAC approach has proven effective in facilitating diagnosis and accelerating the management of children in situations of concern.
Background
Ouaddaï province is located in Eastern Chad on the border with Sudan. It is subject to strong climate fluctuations, rapid desertification, soil erosion and reduced land productivity1 as well as inter-community conflicts leading to internal population displacements. Chad also hosts over 300,000 refugees from Sudan in camps in the Eastern provinces.2 Climatic conditions and migratory flows put great pressure on already weak natural food and financial resources in the Ouaddaï province, as well as on response capacities for the provision of basic social services.
The infant and child mortality rate in Chad is 113 deaths per 1,000 live births which means that one child in ten dies before reaching the age of five years. Leading causes of death are malaria (20.4%), pneumonia (15.7%) or diarrhoea (13.5%)3 with malnutrition being a major contributing factor. In Ouaddaï province in 2018, the prevalence of global acute malnutrition (GAM) was 17.8% and 5.1% for severe acute malnutrition (SAM) (Republic of Chad Ministry of Public Health, 2019). Nutrition interventions in the province therefore have a crucial role to play in ensuring child survival and growth. In its National Nutrition and Food Policy (Republic of Chad, 2013), the Chadian government put in place strategies to improve the nutritional situation including prevention activities and the adequate management of acute malnutrition. The treatment of SAM cases with medical complications is carried out in therapeutic feeding centres (TFC) in district hospitals while cases without complications are treated at the community level in outpatient therapeutic programmes (OTP) attached to Health Centres (HCs).
In 2016, the non-governmental organisation (NGO), Première Urgence Internationale (PUI), began implementing a project to prevent and treat SAM in children under five years of age and pregnant and lactating mothers in Ouaddaï province. In recent years, PUI has identified the need to improve the quality of nutritional care by, among other things, improving the quality and coverage of screening for malnutrition in the community and the referral of children identified for treatment. The ‘Mother-MUAC’ approach involves mothers screening their own children for signs of acute malnutrition using mid-upper arm circumference (MUAC) tapes. The effectiveness of this approach has been demonstrated in Niger (Blackwell et al, 2015) and has been successfully tested in Chad by several NGOs4 as a means of enabling broader and earlier detection of child malnutrition. PUI began incorporating Mother-MUAC within its wasting treatment and prevention programme in Ouaddaï province in 2018, adapting it to the programme realities of the context. This article describes that process, the results and the lessons learned.
Implementation of the Mother-MUAC approach in Ouaddaï province
PUI has been implementing a SAM prevention and treatment programme in an area covered by 24 HCs in the health districts of Adré (11 out of 22 HCs), Abougoudam (four out of 11 HCs) and Abéché (nine out of 30 HCs) in Ouaddaï province since 2016. The decision to provide support to these three health districts was based on a request from the national authorities who had noted that the management of malnutrition was insufficient due to the lack of support from a technical and financial partner. The services of PUI were recruited to improve the quality of existing SAM management services and set up new services where they did not already exist.
Until May 2018, community screenings and referrals of malnourished children aged 6-59 months were carried out by Community Relays (in French, ReCo) - community health agents supervised by the team of around four community health workers (CHWs) from each HC. By this time, PUI had recruited and trained 370 ReCos and 152 CHWs across the three health districts. The ReCos were assigned to a group of villages to carry out malnutrition screening. These screenings were expensive because ReCos and CHWs were paid, with additional bonuses paid on condition of results (number of children screened for malnutrition, proper reporting done, community sensitisation carried out).
From May 2018, several adaptations were made to the programme in response to reduced funding. Firstly, the number of targeted HCs was reduced by three - from 24 to 21. The three HCs with the best performance criteria (programme coverage, quality of care, etc.) were selected for reduction in support services to minimise any negative impacts. In addition, Mother-MUAC screening was introduced as a more financially sustainable form of community screening as well as to support the more rapid identification and referral of children with acute malnutrition for treatment, thereby reducing the complications and mortality associated with late treatment.
In this approach, mothers were trained to identify acute malnutrition, either by using a coloured tape to measure MUAC or by detecting oedema. Mothers were trained to screen their own children as well as other children from within their neighbourhood or village. This is different to the common application of the Mother-MUAC approach whereby each mother only screens her own child. PUI chose to adapt this and train mothers to screen around 12 children aged 6-59 months each, including their own children and others in their village, all in a voluntary, unpaid capacity.
Process for introducing the Mother-MUAC approach
The process of moving from the ReCo screening to Mother-MUAC was implemented over a two-month period in June and July 2018. The main steps in this process are described below.
Informing and mobilising the community around the approach
PUI, together with the District Executive Teams, discussed the approach with HC managers (responsables des centres de santé, RCS), health centre management committees (comités de gestion des centres de santé, COGES) and health committees (comités de santé, COSAN) in each zone to obtain their approval so that they could then sensitise the community on the value of the early detection of acute malnutrition and the role of mothers in the prevention of malnutrition.
Identification of beneficiary villages
In collaboration with community leaders, the RCS, COSAN/COGES and functional women groups in the villages, 759 villages were identified to be part of the programme's coverage area. A total of 201 out of 960 (21%) were excluded as they were small or very small villages. Those comprised a large number of ferricks, villages with only a few households, and nomadic non-permanent settlements.
Identification of the mothers
In order to reach as many mothers as possible, several criteria guided the identification of Mother-MUACs. To become a Mother-MUAC, volunteers were asked to be available and active in their community, be of childbearing age, be accepted by the community, have resided in the village for at least one year and accept doing the screening activity on a voluntary basis.
Training and awareness
In July 2018, mothers were trained on the use of the MUAC tape to screen for malnutrition (MUAC measurement), identification of oedema, effective infant and young child feeding practices and how to refer children identified as having SAM to nutritional management units. All women identified to be Mother-MUAC were grouped in central locations for a one-day training session. Training was conducted by a team comprised of two nurses - one from the RCS and the other a PUI staff member.
Implementation of community-based screening and referral
Following the training, each mother received MUAC tapes and began to screen all children aged 6-59 months in their village/neighbourhood on a monthly basis. Mothers were also given yellow and red coupons to pass on to the caregivers of children identified with acute malnutrition in place of referral forms (yellow if the child was referred for MAM and red if the child was referred for SAM). When a child was identified as having either MAM or SAM, the caregiver was sensitised by the trained mother to transfer the child to the HC for treatment. If the caregiver refused, further sensitisation sessions were held to overcome the barriers preventing the mother taking her child to the HC. When the caregiver of the identified child went to the nutrition unit, she gave the coupon to the health worker who then performed a further assessment to validate (or not) the diagnosis based on admission criteria of the national protocol, i.e., either MUAC or weight-for-height z-score. Transportation costs for the referral were borne by the families.
Follow-up and reporting
Monitoring of the activity was carried out by the CHWs who were already trained and experienced in MUAC screening. Each month, the CHWs summarised the number of children referred via Mother-MUAC at each HC. Each CHW also conducted random MUAC measurements in households covered by the Mother-MUAC programme to ensure the effectiveness of the screening and the reliability of measurements. A monthly review was conducted with the PUI teams. When an area showed low performance, on-site individual training was conducted in order to improve the quality of measurement.
At the health district level, the PUI project team and the CHWs documented the consistency and reliability of the reported MUAC colour and the presence of oedema reported by mothers compared to the result of CHW screening on arrival at the HC.
Performance analysis
In order to analyse the performance of screening and compare the two approaches, PUI analysed the following indicators pertaining to the treatment of children with SAM:
- Screening coverage: number of children screened for MUAC and/or oedema compared to the total number of children in the coverage area.
- Screening performance: based on the number of children identified as having SAM by the mothers, PUI analysed the number of children who were referred, the number of children referred who arrived at the HC and the number of referred children who were confirmed as having SAM at the HC and treated according to the protocol.
- Treatment performance indicators: based on the number of children who exited the programme, those that exited as cured, dropped-out, died or non-recovered were recorded from both inpatient care and OTCs.
- Mothers' ownership of the activity: the perceptions of mothers around the approach were collected informally by the project managers during the monitoring of the implementation.
Feedback from HC staff was also sought which provided informal yet key feedback on programme implementation.
Programme achievements
From May 2018 to December 2019, 15,004 mothers were identified and trained in the areas of responsibility of 21 HC in the three health districts of Adré, Abougoudam and Abéché.
Screening coverage
Of the 77,920 children aged 6-59 months expected for the period, a total of 66,613 were screened using the Mother-MUAC approach, representing a coverage rate of 85.5% in 21 areas of responsibility.5 Over the same period during the previous year (using the CHW-ReCos screening approach), 76,710 children were screened of the 96,417 children expected, with a coverage rate of 79.5% across 24 areas of responsibility (Figure 1).
Figure 1: Screening coverage according to approach (Mother-MUAC vs. ReCo/CHW)
| Mother-MUAC | ReCo/CHW | |
| # Children expected in coverage area | 77, 920 | 96, 417 |
| # Children screened | 66, 613 | 76, 710 |
| Screening coverage | 85.5% | 79.6% |
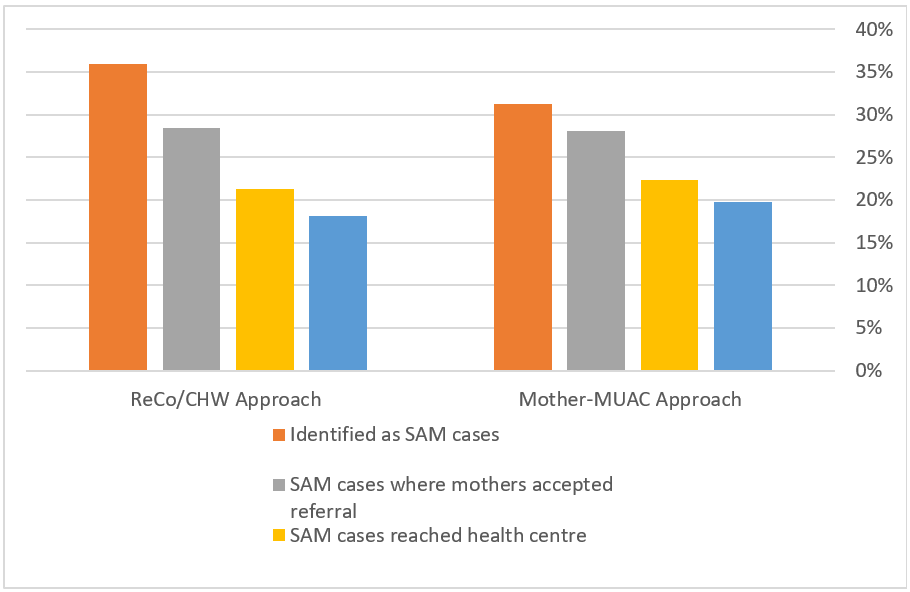
Screening performance
The Mother-MUAC approach identified 22,791 malnourished children including 15,812 cases of MAM6 (23.7% of the children screened) and 6,979 cases of SAM (10.5% of the children screened). Of the SAM cases detected, 6,271 (89.8%) were SAM cases where mothers accepted referral to a nutritional care unit, 4,971 (71.2% of the SAM cases detected) arrived at a HC supported by PUI and 4,413 (63.2% of the SAM cases detected) were actually admitted for treatment (Figure 2). Therefore, 63.2% (two out of three) of all children identified as having SAM by the mothers were confirmed as having SAM at an HC and treated following the protocol. In comparison, screening by CHWs and ReCos during the previous phase of the project7 identified 37,448 malnourished children including 13,471 cases of SAM, among whom 6,767 (or 50.2%, or half) were admitted to a nutritional care unit for treatment.
Figure 2: Screening performance (Mother-MUAC vs. ReCo/CHW)
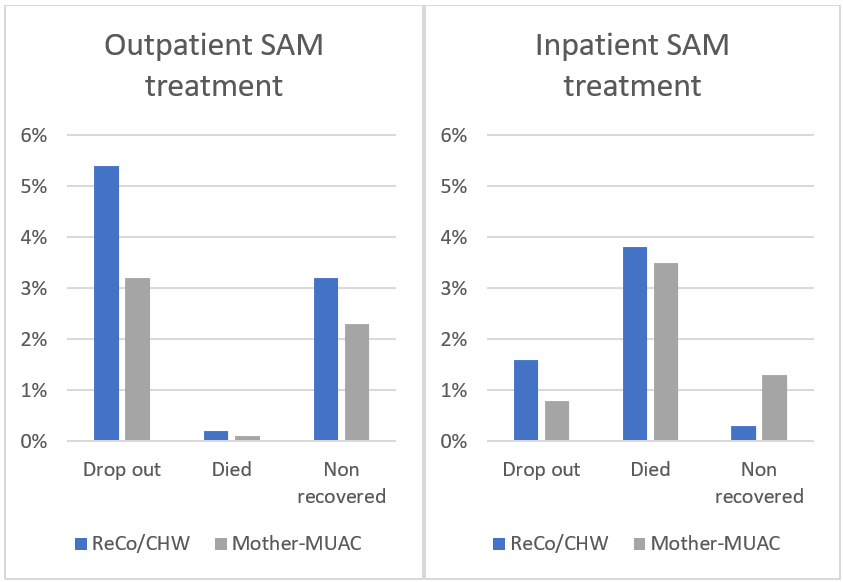
Therapeutic treatment performance indicators
The cure rate in OTCs was higher in 2019 (95%) after transitioning to the Mother-MUAC approach than before (91.5%). The cure rate in inpatient care was not significantly different, a little over 94% for both approaches. Other performance indicators (exited from the programme as dropped-out, died or non-recovered) improved with the implementation of the Mother-MUAC approach (Figure 3).
Figure 3: Treatment performance indicators (Mother-MUAC vs. ReCo/CHW)
Ownership of the activity by the mothers
Analysis of mothers’ perceptions of the effectiveness of screening through the Mother-MUAC approach were carried out through 60 sessions supervised by the PUI Health Supervisors and the ReCos. These sessions revealed strong participation of mothers in the management of their child's health and a strong sense of ownership of the activity that they carried out on a voluntary basis. The involvement of mothers in malnutrition screening allows them to better understand the signs of malnutrition, to participate in monitoring the nutritional status of their children and increases the frequency of screening of children at the community level.
Nevertheless, 29% of children identified as having SAM by the mothers never arrived at a HC unit. Discussions revealed that the common causes for caregivers not taking referred children to a HC were the long distances to be covered, the natural barriers in the form of ouadis in the rainy season (temporary watercourses making access impracticable), mothers' refusal to be referred or a lack of authorisation from their husbands and the heavy workload of mothers making them unavailable (other household chores or work in the fields). The implementation and monitoring of this approach helped to strengthen community support and facilitate acceptance of the programme in the area. Moving forward, additional efforts will be made to improve compliance with referrals, such as intensifying sensitisation (including targeted at men) and the strengthening of a community solidarity fund, managed by COGES, to provide financial aid to families that are not able to afford the transportation costs.
Health Centre staff feedback
Interviews with HC staff indicated their perception that, as a result of the training of mothers on the Mother-MUAC approach, there is better programme coverage and mothers/children's carers are more cooperative with treatment protocols and less likely to default. There is evidence that the radius of coverage was extended beyond 15km from most HCs, a radius that CHWs and ReCos never exceeded due to a lack of transport available to access remoter villages.
Discussion and conclusions
Screening for acute malnutrition at the community level is often the responsibility of CHWs. However, there is growing evidence that families, especially mothers, can play an important role in screening for acute malnutrition through the measurement of their child’s MUAC and for signs of oedema in their own communities. In the context of this programme, the Mother-MUAC approach provided better coverage of screening than the CHW-ReCo approach and a higher screening performance, demonstrated by the higher percentage of SAM children identified by mothers being admitted for treatment at an HC (63.2% in the Mother-MUAC approach versus 50.2% in the CHW-ReCo approach). There is some indication that this has led to shorter treatment duration which suggests that children are being referred more quickly for treatment, thereby potentially reducing malnutrition-related morbidity and mortality.
Results also demonstrate strong acceptance by mothers of the Mother-MUAC approach, both by mothers doing the screening and by mothers whose children are being screened by mother-peers. HC staff are also highly supportive of the approach, due to the improved programme coverage and the cooperation of caregivers. In addition, compared to the CHWs-ReCos approach, the Mother-MUAC approach has reduced the programme support costs by 27%, according to average support cost per HC. Given the lack of funding and the need to ensure regular community screening, the Mother-MUAC approach is proving to be a sustainable approach in this context. The motivation of the mothers is not financial which allows for its sustainability, replicability and scaling up at the national level.
Community-based screening has shown that more regular and earlier detection could reduce the risk of mortality and morbidity in children 6-59 months of age. In our experience, the Mother-MUAC approach has proven effective in facilitating diagnosis and accelerating the management of children in situations of concern. The implementation process is relatively straightforward and empowers mothers to be actors in the health of their children. Regular monitoring of the mothers' activity and good supervision promote control over MUAC measurements.
Although the impacts of COVID-19 were not a major issue in PUI’s programme area and did not modify the attendance rate at HCs, appropriate steps were taken to enforce proper prevention measures and to support newly formed epidemic surveillance committees.
Looking ahead, PUI aims to continue supporting the management of acute malnutrition in this area while working towards handing over activities to the government structures and expanding its activities to better address the underlying causes of malnutrition. With the support of the 11th European Development Fund, and in partnership with a local NGO, this new phase will focus on increasing agricultural production while also working towards more preventive nutrition activities, including improving infant and young child feeding practices.
For more information, please contact Chantal Autotte Bouchard at cautottebouchard@premiere-urgence.org.
1 Climate vulnerability index https://www.maplecroft.com/
4 The Mother-MUAC approach is being used in Chad by the NGOs: Action contre la Faim, International Rescue Committee and ALIMA.
5 Children are screened on a weekly basis but counted only once.
6 PUI only supported SAM treatment programmes. Children with MAM were therefore not tracked under this programme.
7 The first phase of the project covered a larger geographic area, thus the greater number of children expected.
References
Blackwell, N, Myatt, M, Allafort-Duverger, T, Balogoun, A, Ibrahim, A and Briend, A (2015) M others U nderstand A nd C an do it (MUAC): a comparison of mothers and community health workers determining mid-upper arm circumference in 103 children aged from 6 months to 5 years. Archives of Public Health, 73(1), 26.
Institut national de la statistique des études économiques et démographiques (INSEED) (2016) Enquête démographique et de santé et à indicateurs multiples au Tchad (EDS-MICS), 2014-2015. Rockville, Maryland, USA : ICF International.
République du Tchad (2013) Tchad: Politique nationale de nutrition et d’alimentation 2014 - 2025.
République du Tchad - Ministère de la santé publique (2019) Enquête nationale de nutrition, TCHAD 2019. Available at: https://reliefweb.int/sites/reliefweb.int/files/resources/rapport_final_enquete_smart_27112019.pdf
More like this
FEX: In Chad, the Mother-MUAC approach improves treatment access for malnourished children
This is a summary of a Field Exchange field article that was included in issue 65. The original article was authored by Hyppolite Gnamien, Chantal Autotte Bouchard, Jean-Robert...
FEX: Au Tchad, l’approche maman-PB permet d’améliorer l’accès des enfants malnutris à un traitement
Read an English version of this article here Par Hyppolite Gnamien, Chantal Autotte Bouchard, Jean-Robert Bwanaissa Shabani, Abdoulaye Mohamed, Emily Helary et Marion...
FEX: Mothers understand and can do it (MUAC)
Summary of research1 Location: Niger What we know: Community based management of SAM often relies on anthropometric screening by Community Health Workers. Training includes...
en-net: Simplified Approaches in the context of COVID 19 (questions escalated to the GTAM Wasting TWG)
a. What can we do to quickly communicate that this [simplified approaches] is an acceptable adaptation to make in the circumstances to enable governments to make this...
FEX: Management of severe acute malnutrition by community health workers: Early results of Action Against Hunger research
View this article as a pdf Lisez cet article en français ici By Pilar Charle-Cuellar, Noemi Lopez-Ejeda, Magloire Bunkembo, Abdias Ogobara Dougnon and Hassane Toukou...
FEX: SQUEAC in routine monitoring of CMAM programme coverage in Ethiopia
By Lily Schofield, Selome Gizaw Lalcha and Terefe Getachew Lily Schofield has worked in many countries in Africa and Asia as a nutrition consultant. She has been involved in...
FEX: Key findings from the Click-MUAC Project
Summary of presentation1 View this article as a pdf By Angeline Grant, Zvia Shwirtz, James Njiru, André Briend and Mark Myatt Angeline Grant is Senior Nutrition and...
FEX: Upcoming research shared at ACF research conference
At the ACF research conference, November 6th, 2016, experiences were shared from a number of studies where final results will be made available in 2017. A snapshot of what to...
FEX: Enabling low-literacy community health workers to treat uncomplicated SAM as part of community case management: innovation and field tests
By Casie Tesfai, Bethany Marron, Anna Kim and Irene Makura Casie Tesfai is a Nutrition Technical Advisor at the International Rescue Committee in New York, where she provides...
FEX: Call for experiences on mothers measuring MUAC
News Are you using the mothers measuring mid upper arm circumference (MUAC) approach or do you know someone who is? If so, we want to hear from you! Action Against Hunger,...
FEX: Community case management of severe acute malnutrition in southern Bangladesh
Summary of study1 Bangladesh has the fourth-highest number of children (approximately 600,000 at any one time) suffering from severe acute malnutrition (SAM) in the world....
en-net: Mother's using MUAC : Results of a large-scale trial
Here is an Archives of Public Health report on a large-scale trial comparing screening by CHWs and mothers for SAM using MUAC. The conclusion is that mothers were not inferior...
FEX: Community health worker-led treatment for uncomplicated wasting: insights from the RISE study
This is a summary of a Field Exchange field article that was included in issue 64. The original article was authored by Bethany Marron on behalf of the RISE study...
FEX: Community health worker-led treatment for uncomplicated wasting: insights from the RISE study
View this article as a pdf Lisez cet article en français ici By Bethany Marron on behalf of the RISE study consortium Bethany Marron is a nutrition advisor and former...
FEX: A series of three related published papers share findings regarding quality of care, treatment outcomes and cost-effectiveness of uncomplicated SAM treatment delivered by community health workers (CHWs) in rural Mali.
By Eleanor Rogers, Karen MartÃnez, Jose Luis Alvarez Morán, Franck G. B. Alé, Pilar Charle, Saul Guerrero, Natalie Sessions and Chloe Puett Quality of...
Scaling up a community-based nutrition package in Afghanistan to improve complementary feeding practices in children 6-23 months of age
View this article as a pdf Click here to listen to an interview with the author on the ENN podcast channel Dr Mohammadullah Noorzad is the Senior Officer for the Community...
FEX: MUAC alone admission to SAM treatment in Bangladesh
Summary of research1 Location: Bangladesh What we know: MUAC and weight-for-height z score (WHZ) are common anthropometric criteria to diagnose severe acute malnutrition...
en-net: Phone-based screening/ early detection of wasting (escalated question to the Wasting TWG)
Phone-based screening/ early detection - where family/ mothers' MUAC is not possible, can mobile-phone based SAM/MAM screening questions be used to identify malnourished...
FEX: Addressing acute malnutrition in Cameroon during an emergency: Results and benefits of an integrated prevention programme
View this article as a pdf Lisez cet article en français ici By Eveline Ngwenyi, Mica Jenkins, Nicolas Joannic and Cécile Patricia Eveline Ngwenyi is a...
en-net: Where is MUAC used as the only admission criteria for SAM treatment programmes?
The CMAM Forum is currently mapping out all programmes where MUAC is used as the only admission criteria for SAM treatment, along with bilateral pitting oedema (as opposed to...
Reference this page
Hyppolite Gnamien, Chantal Autotte Bouchard, Jean-Robert Bwanaissa Shabani, Emily Helary and Marion Blanloeuil (). In Chad, the Mother-MUAC approach improves treatment access for malnourished children. Field Exchange 65, May 2021. p22. www.ennonline.net/fex/65/mothermuacapproachchad
(ENN_7041)