Bangladesh: The rationalisation of nutrition services in Rohingya camps
This article outlines the provision of nutrition services in Cox’s Bazar, an area where multiple partners work together to deliver to those in need in the refugee population. At times, this can result in duplication, double counting and gaps in service provision.
Bakhodir Rahimov is a Nutrition Sector Coordinator in Cox’s Bazar, Bangladesh working with UNICEF
Abid Hasan is an Information Management Officer in Cox’s Bazar, Bangladesh
Karanveer Singh is a paediatrician and Nutrition Manager for UNICEF Cox’s Bazar office, Bangladesh
Piyali Mustaphi is Chief of the Nutrition Section in UNICEF’s Bangladesh Country office
Jannatul Ferdous Shoshi is an Emergency Nutrition Officer for the Nutrition Sector in Cox’s Bazar, Bangladesh. She has over five years’ experience in nutrition programming
Mohammed Lalan Miah is the Nutrition Surveillance Head of Department for Action Against Hunger Bangladesh. Mohammed Miah also leads the Nutrition Sector Assessment and Information Technical Working Group.
The authors acknowledge all sector partners' kind contributions to the work described in this article. Sector partners include the Government of Bangladesh, United Nations programme partners (namely, the World Food Programme, UNICEF and the United Nations High Commissioner for Refugees), international and Bangladesh non-governmental organisations, donors and other nutrition sector members in Cox's Bazar. Special thanks to all site supervisors of the integrated nutrition facilities for adopting the COVID-19-modified nutrition protocols and for continuing to run the facilities despite the challenges brought about by the COVID-19 pandemic.
Location: Bangladesh
Key Messages:
- In 2019, nutrition sector partners proposed and conducted a nutrition service rationalisation process. As a result, since January 2020, all nutrition services in each camp are provided through integrated nutrition facilities with a complete package of globally recommended nutrition services for children under five years of age and pregnant and lactating women.
- When exploring the impact of this process, coverage of nutrition screening increased from 66.4% to 93.8% from 2018 to 2020 while prevalence of severe wasting deceased. Programme quality data (as evidence through cure and death rates) did not show any negative impact and defaulter rates reduced substantially
- As a next step for this work, an evaluation will be conducted to explore the qualitative impact of the rationalisation process, both on service providers and beneficiaries.
Background
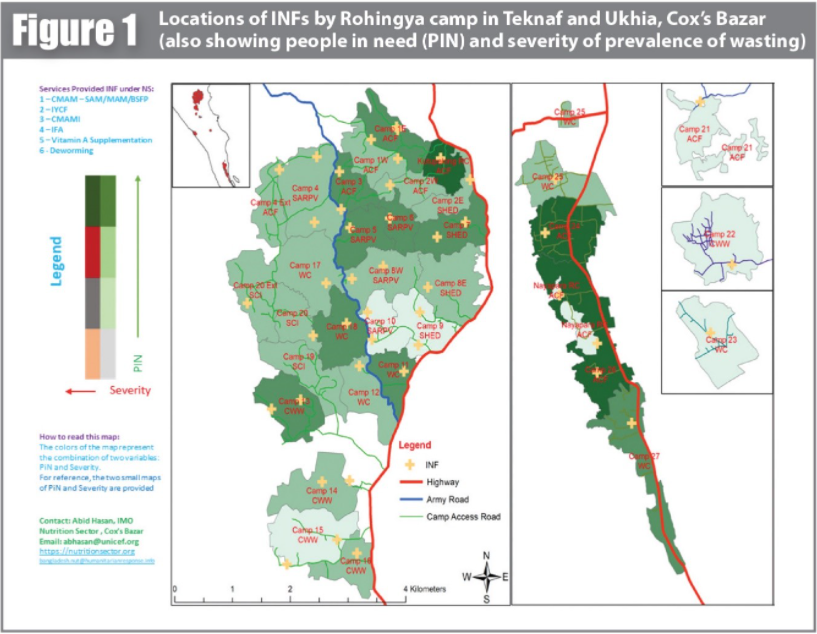
Cox's Bazar District currently hosts over 889,400 Rohingya refugees, nearly all of whom live in 34 congested refugee camps.1 Out of the total population, there are 160,544 children under five years of age, 124,517 adolescent girls (10-19 years old) and 42,000 pregnant and lactating women (UNHCR, 2020). Guided by the Humanitarian Needs Overview (HNO) and Joint Response Plan (JRP), multiple partners work together to provide nutrition services to those in need in the refugee population, coordinated by the Government of Bangladesh and the UNICEF co-led nutrition sector. Since 2020, all nutrition services have been provided through 46 integrated nutrition facilities (INF), including outpatient therapeutic programmes (OTP) for the treatment of severe wasting, targeted supplementary feeding programmes (TSFP) for the treatment of moderate wasting and blanket supplementary feeding programmes (BSFP). In addition, maternal, infant and young child feeding (MIYCF) counselling is provided through these nutrition facilities, using both one-on-one and small group sessions (adhering to social distancing regulations and broader modifications as a result of the COVID-19 pandemic). Adolescent girls and pregnant and lactating women (PLW) are targeted with iron and folic acid (IFA) supplementation. Vitamin A supplementation campaigns for children under five years of age are run in the camps twice a year.
Annually, nutrition sector partners provide OTP services to almost 12,000 children under five years of age with severe wasting and TSFP services to over 46,000 children under five years of age with moderate wasting. In addition, over 145,000 children under five years of age and 42,000 PLW are reached with BSFP monthly. The anaemia prevention programme distributes IFA to 112,000 adolescent girls and 38,000 PLW. The MIYCF counselling sessions reach almost 3,000 PLW, mothers and caregivers of children under five years of age monthly.
Nutrition service arrangements
Prior to 2019 and the nutrition sector rationalisation process, there were 84 scattered OTP, TSFP and BSFP programmes in the camps. Nutrition services were supported by different United Nations (UN) agencies and implemented by different implementing partners (non-governmental organisations (NGOs)) with the location of these partnerships across camps scattered and, in some cases, illogical with catchment areas not clearly defined. This resulted in gaps, overlaps and duplication in both the provision of services and in reaching targeted beneficiaries. The nutrition sector partners therefore proposed a nutrition service rationalisation process which was completed by the end of 2019.
As a result, since January 2020, all facilities and partnerships providing nutrition services are split by camp with a single INF providing a complete package of globally recommended nutrition services for children under five years of age and PLW through a ‘one-stop shop’ with community-based management of acute malnutrition (CMAM) (OTP and TSFP) and MIYCF services at the core. The nutrition sector maintains at least one INF per camp, with some camps having a satellite nutrition facility to serve larger catchment populations, resulting in a total of 46 INFs across the 34 Rohingya camps (Figure 1). INFs are coordinated and managed by the site supervisors and respective NGO staff who report to the nutrition sector as per the HNO and JRP targets.
This article describes the early results of the nutrition service rationalisation process, the observed challenges and the lessons learnt to demonstrate the utility of this approach in terms of coverage and the overall performance of nutrition services.
The process of nutrition service rationalisation
The nutrition service rationalisation process was long and, at times, difficult. It required a strong commitment from UN, government and implementing (NGO) partners to cooperate and work together. Nutrition sector meetings were the platform for discussions and communication on the rationalisation process between all stakeholders. As a first step, all UN partners had to agree to retain only one nutrition site in each camp, with the largest nutrition facility within each camp selected to bring all nutrition services under a single roof. Nutrition services at smaller centres discontinued and these facilities were repurposed for other activities, including storage.
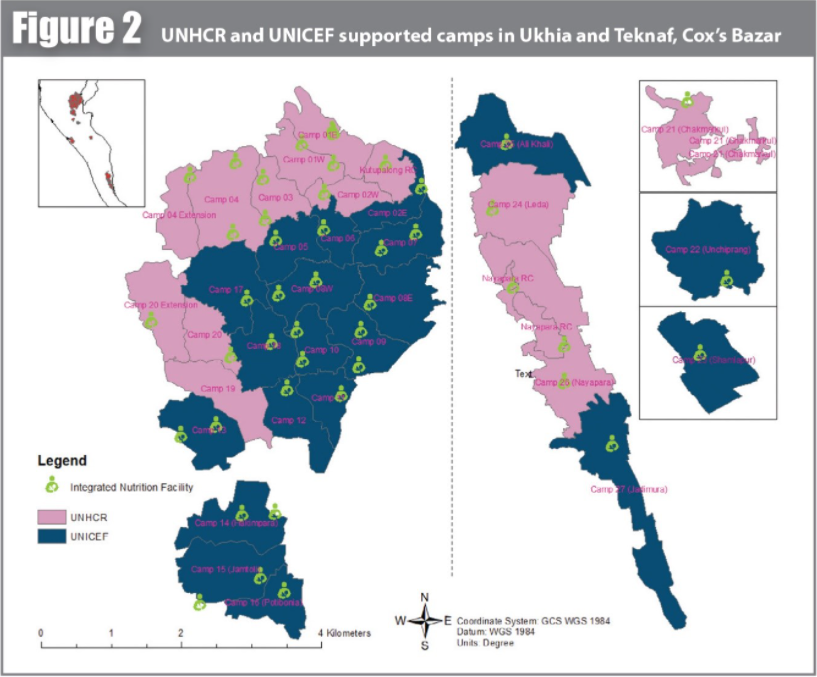
As the World Food Programme (WFP) was the only UN partner supporting TSFP and BSFP activities, they continued to provide these nutrition services in all camps. For OTP services, UNICEF and the United Nations High Commissioner for Refugees (UNHCR) geographically split the locations based on agreed criteria including the average estimated cost of running the nutrition facility combined with the respective UN agencies’ annual budget and the number of active partnerships with implementing partners (Figure 2). As a result of this process, WFP supports all 34 camps with TSFP and BSFP services while UNHCR supports 14 camps and UNICEF supports 20 camps with OTP services.
Implementing partners were allocated to each INF through mutual agreement depending on their experience, existing capacity and the financial resources available. The final documentation outlining who would be responsible for what service and where was initiated by the implementing partners, submitted to the nutrition sector and finally approved by the Refugee, Repatriation and Relief Commissioner in Cox’s Bazar.
A more complete process of the nutrition service rationalisation process will be described in future Field Exchange publications once the process has evolved further.
Programmatic results of the nutrition service Programmatic results of the nutrition service rationalisation process
To understand the direct and indirect impact of the nutrition service rationalisation process, we compared the coverage of nutrition services and the key performance indicators from 2018 to 2020. The key indicators used to assess coverage and performance (Box 1) are drawn from nutrition sector reports.2 The results are provided in Table 1.
Box 1: Indicators used to assess coverage and performance
-
Proportion of children under five years of age screened for malnutrition (out of the total number of children under five years of age in the camp population per year).
-
Proportion of wasted children (severe and moderate) out of the total number of children screened per year.
-
The proportion of cured, defaulted or deceased cases among children under five years of age admitted in CMAM programmes.
-
Average number of MIYCF counselling sessions received by caregivers of children classified as being wasted.
Table 1: Comparison of CMAM and MIYCF programme indicators by year
|
Indicators |
2018-2020 average |
2018 |
2019 |
2020 |
|
Proportion of children screened for wasting |
72.6% |
66.4% 95% CI 61.6-71.69 |
57.7% 95% CI 50.45-64.86 |
93.8% 95% CI 78.84-108.77
|
|
Proportion of children identified and admitted with severe wasting out of total number of children screened |
1.6% |
2.4% 95% CI 1.91-2.83 |
1.7% 95% CI 1.34-2.03 |
0.6% 95% CI 0.46-0.72 |
|
Proportion of children identified and admitted with moderate wasting out of total number of children screened |
2.9% |
3.0% |
2.8% |
3.0% |
|
Cure rate among children with severe wasting in CMAM programme |
92.7% |
96.6% |
91.1% |
90.3% |
|
Default rate among children with severe wasting in CMAM programme |
1.0% |
1.9% |
0.7% |
0.4% |
|
Death rate among children with severe wasting in CMAM programme |
0.2% |
0.1% |
0.2% |
0.2% |
|
Cure rate among children with moderate wasting in CMAM programme |
86.6% |
78.4% |
90.1% |
91.2% |
|
Default rate among children with moderate wasting in CMAM programme |
6.2% |
14.6% |
3.2% |
0.7% |
|
Death rate among children with moderate wasting in CMAM programme |
0.2% |
0.1% |
0.2% |
0.5% |
|
Average number of MIYCF counselling sessions for caregivers of children with severe wasting |
|
1* |
3.0 |
4.9 |
|
Average number of MIYCF counselling sessions for caregivers of children with moderate wasting |
|
1* |
2.3 |
1.4 |
* 2018 is taken as a baseline and compared with the following results in 2019 and 2020. For example, counselling sessions for the caregivers of children with severe wasting were given 4.9 times more than in 2018.
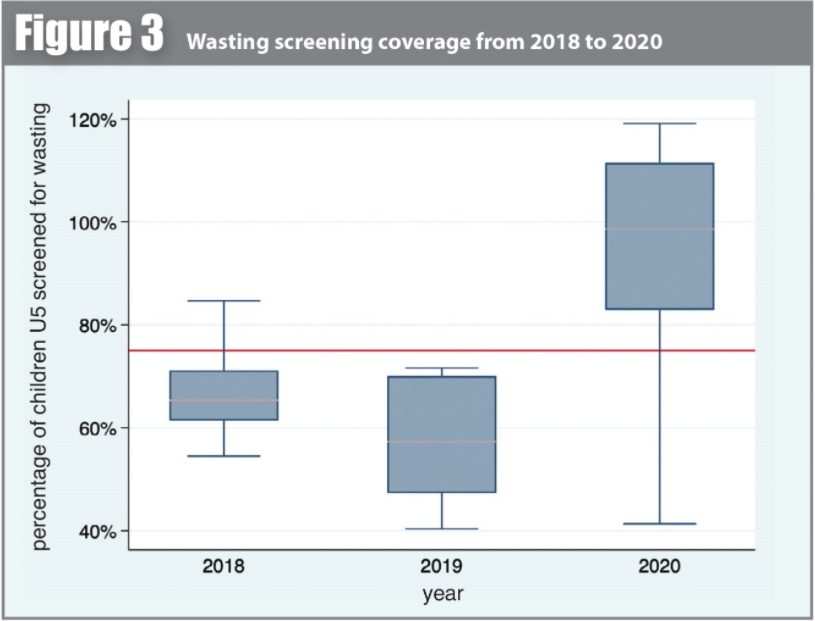
Coverage of wasting screening
Between 2018 and 2020, the geographic coverage of community wasting screening increased from 66.4% to 93.8% despite a drop to 57.7% in 2019 – a year when the sector partners worked to avoid duplicating services and counting the same beneficiaries at multiple sites (known as double counting). Almost all children under five years of age were reached for wasting screening following the nutrition service rationalisation process (Figure 3).
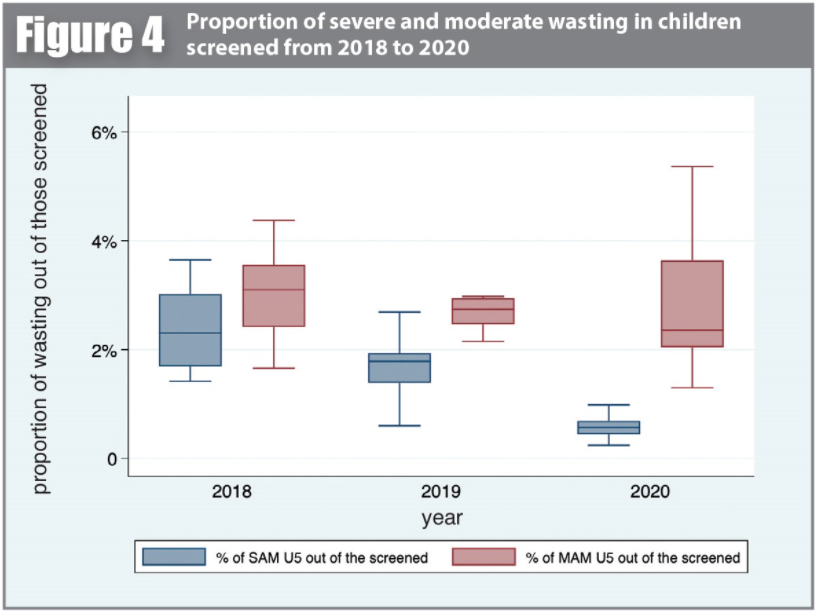
Proportion of wasted children out of those screened
Among children under five years of age screened for wasting, the proportion of those identified with severe wasting reduced considerably from 2.4% in 2018 to 0.6% in 2020. However, the proportion of children under five years of age screened and identified with moderate wasting did not vary from before and after the nutrition service rationalisation. It remained at around 3% in 2020, the same proportion reported in 2018 (Figure 4).
CMAM programme performance indicators
CMAM programme performance indicators (cure, defaulter and death rates) either improved or remained stable following the nutrition service rationalisation. The cure rates for children treated for either severe or moderate wasting were consistently above the recommended Sphere standard of 75%. In relation to severe wasting cure rates, comparisons from 2018 to 2020 showed a slight decrease from 96.6% in 2018 to 90.3% in 2020 while moderate wasting cure rates increased during the same time period from 78.4% in 2018 to 91.2% in 2020. Defaulter rates reduced in OTPs from 1.9% in 2018 to 0.4% in 2020 and in TSFPs from 14.6% in 2018 to 0.7% in 2020. Death rates for children treated for either severe or moderate wasting were also consistently lower than Sphere standards at less than 1% across the three-year time period. This appeared to be relatively independent of seasonal influences and other emergencies such as the COVID-19 pandemic.
MIYCF counselling
The coverage of the MIYCF counselling programme increased with the rationalisation of nutrition services. The number of counselling sessions held with caregivers of children with severe wasting (either through group sessions or one-on-one counselling) increased almost five-fold from an average of one session in 2018 to 4.9 sessions in 2020. This takes into account the exclusion of double counting after service rationalisation. However, MIYCF counselling sessions given to caregivers or mothers of moderately wasted children showed a different picture. The average number of MIYCF counselling sessions received increased to 2.3 times that of 2018 in 2019 but in 2020 was only 1.4 times that of the 2018 rates.
Discussion
The nutrition service rationalisation led to many improvements in nutrition service provision in Cox’s Bazar. The double counting of beneficiaries and the duplication of services were reduced, as indicated by the improved coverage of nutrition screening and reduced defaulter rates. Beneficiary convenience was increased as there was no longer a need to search for appropriate nutrition services at a number of different facilities. Overall, the demarcation of the UN partners’ programmatic accountability by camp increased the level of emergency preparedness and responsiveness as implementing partners felt more ownership of nutrition services in their allocated locations. It also prevented the duplication of financial resource allocation from different agencies for the same services and activities.
The proportion of children identified with severe wasting dropped significantly from 2018 to 2020 which is likely due to the improved performance of the INFs and increased community screening within the catchment population, as well as the timely adoption and dissemination of COVID-19 CMAM protocol modifications for earlier identification of cases of wasting. The proportion of children with moderate wasting did not decrease over the same time period which calls for an increased need to focus efforts on the prevention, as well as treatment, of wasting moving forward. Treating moderate wasting effectively with a good level of coverage would lead to a reduction in the prevalence of severe wasting but ultimately comprehensive context-specific prevention of wasting services are needed to reduce the overall prevalence of wasting.
It appears that the rationalisation process did not negatively impact nutrition service quality. Looking at CMAM programme performance indicators, all three indicators (cure, defaulter and death rates) provide evidence of sustained high-quality OTP and TSFP services throughout the pandemic and the rationalisation process. However, MIYCF programme coverage for children admitted to the TSFP programme fell in 2020 although this is likely a direct result of nutrition protocol modifications in response to the COVID-19 pandemic rather than as a result of the rationalisation process. The MIYCF programme shifted from group to individual sessions and prioritised counselling in OTPs rather than TSFPs. There is a need to refocus efforts on MIYCF counselling for cases of moderate wasting moving forward as COVID-19 restrictions are eased.
Adaptations to the COVID-19 pandemic
The nutrition service rationalisation process proved very timely as it was implemented shortly before the onset of the COVID-19 pandemic. Due to COVID-19, restrictions on moving staff in and out of camps were imposed resulting in available staff numbers being reduced by over half. Having integrated and rationalised services allowed the nutrition sector to continue to provide all services (OTP, TSFP and BSFP) despite the reduced staff numbers. Furthermore, as a result of limited access to the camps, sector partners engaged in a process of building the nutrition capacity of Rohingya nutrition volunteers, particularly in relation to the screening of children. This has enabled more sustainable and community-led programming as a result.
COVID-19 modifications to the nutrition protocol were also put into place, including expanding mid-upper-arm circumference (MUAC) cut offs and rolling out the mother-led MUAC approach (Dube et. al., 2020; Miah et al., 2020). While comparisons between 2018 and 2020 do not reflect these changes, it was noted that these adaptations had a substantial impact on admissions to nutrition services from March 2020 (Dube et. al., 2020). From May 2020, the nutrition sector implemented the mother-led MUAC approach and, since then, over 130,000 caregivers and mothers of children under five years of age have been trained in the use of MUAC.
Limitations
We were not able to analyse the cost-efficiency of the rationalisation process due to the limited availability of financial information. It would be interesting to explore the cost benefits of such a process and understand the financial and human resource implications of the rationalisation process. Broadly speaking, the process did not appear to result in any additional needs and this was demonstrated by the COVID-19 pandemic requiring no further human or financial resources from the nutrition sector, yet quality of programming was still maintained. However, accurate data on this would be useful to inform similar exercises in other contexts.
Another limitation to this process was the lack of qualitative data on the impact of the rationalisation. While the quantitative data available highlights positive impact, it would be valuable to understand more about the nuances of the process and the feedback of those involved as well as the beneficiaries. With funds received from European Civil Protection and Humanitarian Aid Operations in 2021, the nutrition sector is planning to conduct an evaluation of the nutrition sector response in the Rohingya camps. The evaluation will focus on beneficiaries and service providers’ perceptions of the quality and comprehensiveness of nutrition services before and after the sector rationalisation. The qualitative results of the evaluation will be compared and combined with the quantitative results outlined in this article. The authors plan to summarise and publish these combined findings in a subsequent article in Field Exchange.
Conclusion
Only one year has passed since the introduction of the nutrition service rationalisation. The sector partners aim to continue documenting and reporting the changes resulting from the rationalisation process and reflect on the lessons learnt. Programmers in humanitarian and development contexts should consider conducting a nutrition service rationalisation process to bring all nutrition services together under one roof given the positive impact relating to programme coverage and service quality. The concept of a ‘one-stop-shop’ is not new but only a limited number of countries have restructured nutrition services and united OTP, TSFP and BSFP programmes together. Nutrition service rationalisation is recommended as it not only provides an opportunity to integrate health and nutrition services, it also supports a disability-friendly environment and allows the mainstreaming of gender and protection services through a single programme.
For more information, please contact Bakhodir Rahimov at brahimov@unicef.org
References
Choudhury N, Tahmeed A, Iqbal MH, Mandal B, Mothabbir G, Rahman M et al (2014) Community-Based Management of Acute Malnutrition in Bangladesh: Feasibility and Constraints. Food and Nutrition Bulletin, 35, 2, 277–85.
Dube T, Koech C'at M, Mustaphi P, Harlass S, Singh K & Bourdaire, J (2020) Adaptations to CMAM Programming in Cox’s Bazar in the Context of the COVID-19 Pandemic. Field Exchange 63, ENN 57. www.ennonline.net/fex/63/cmamcxbcovid19adaptations.
IPHN (2017) Bangladesh National Guidelines for Community Based Management of Acute Malnutrition. IPHN. https://www.humanitarianresponse.info/en/operations/bangladesh/document/national-guidelines-community-based-management-acute-malnutrition.
Miah ML, Rahman M & Sarker, B (2020) Concordance between Weight-for-Height z-Score (WHZ) and Mid-Upper Arm Circumference (MUAC) for the Detection of Wasting among Children in Bangladesh Host Communities. Field Exchange 63, 81. www.ennonline.net/fex/63/whzmuacbangladesh.
1 UNHCR (2020) Population estimate for the Rohingya camps. Situation Refugee Response in Bangladesh (unhcr.org) https://data2.unhcr.org/en/situations/myanmar_refugees
2 Reports were drawn from the 4W platform. 4W is a reporting tool of the Joint Response Plan (JRP) under the general coordination of the Inter-Sector Coordination Group (ISCG) in Cox’s Bazar. 4W reports were compiled monthly and consolidated in the annual JRP monitoring and reporting frameworks.


