Nutrition Impact and Positive Practices (NIPP) in Sudan
Marlene Hebie is a roving Nutrition Advisor at GOAL Global.
Sarah Ibrahim Mohammed Nour is a Nutrition Coordinator at GOAL Sudan.
Hatty Barthorp is a Global Nutrition Advisor at GOAL Global.
This article is based on an independent evaluation commissioned by GOAL and led by Action Against Hunger UK’s Monitoring, Evaluation and Learning Services, through support from the U.S. Agency for International Development (USAID). We acknowledge the contribution of Joel Woolfenden, a member of the Action Against Hunger evaluation team, in an early version of this paper. Since its inception, NIPP has been funded in Sudan, South Sudan, Niger, Malawi, Zimbabwe and Uganda by Irish Aid, the UK Foreign, Commonwealth and Development Office, ECHO, the Office of Foreign Disaster Assistance, USAID, the Sudan Humanitarian Fund managed by the United Nations Office for Coordination of Humanitarian Affairs, UNICEF, the United Nations High Commissioner for Refugees, the Garden Trust and the Waterloo Foundation.
Background
Despite some progress, maternal and child malnutrition remains a global health concern, worsened by the COVID-19 pandemic. In Sudan, 37% of children under five years of age suffered from stunting and 17% from wasting in 2019 (UNICEF, 2019). In addition, according to UNICEF and the World Health Organization thresholds (de Onis, 2018), 14 out of 18 (82%) states in Sudan had a very high prevalence of stunting (≥30%) and 11 out of 18 (61%) a very high prevalence of wasting (≥15%). The burden of malnutrition is partly driven by inadequate maternal, infant and young child feeding (M-IYCF) practices and inappropriate hygiene, sanitation and health seeking behaviours (UNICEF, 2019). This situation is exacerbated by the protracted humanitarian crisis in conjunction with El Niño-associated food insecurity and malnutrition. Tackling malnutrition is one of the core challenges of the 21st century (Development Initiatives, 2018) and involves addressing many complex and inter-related determinants.
The Nutrition Impact and Positive Practice approach
GOAL in Sudan (GS) has been implementing health and nutrition programming in Kutum locality, North Darfur state since 2004 in response to the humanitarian crisis. GOAL’s approach encompasses health system strengthening to support the provision of integrated therapeutic nutrition services and M-ICYF alongside a preventive component through the Nutrition Impact and Positive Practice (NIPP) approach.
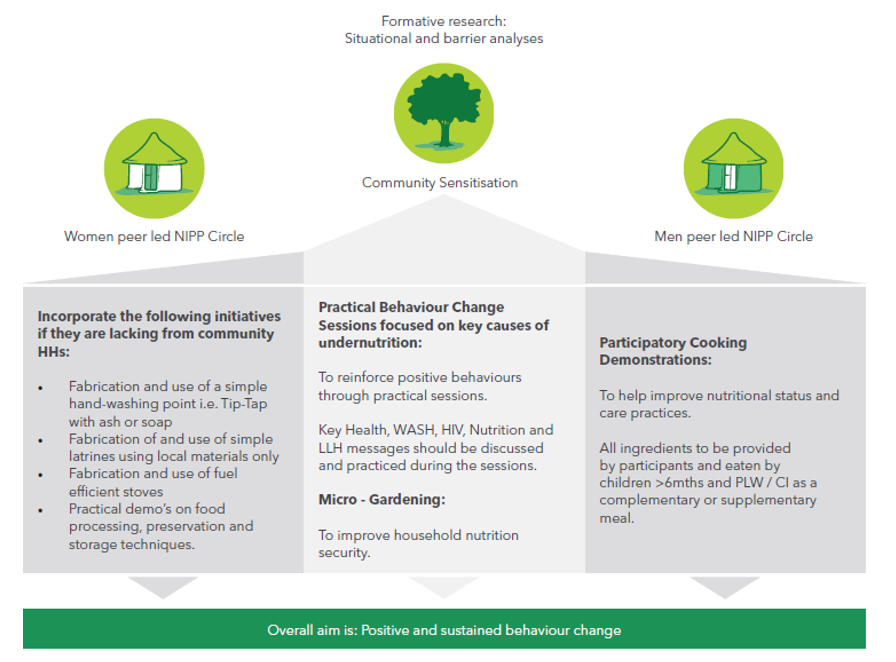
The NIPP approach was designed by GOAL in 2012 as a gender sensitive, multi-sector, grass-roots programme to address the behavioural determinants of malnutrition. The approach involves a 12-week series of meetings during which community leaders and separate groups of male and female caregivers participate in practical behaviour change sessions to tackle the issues contributing to malnutrition in their community. Participation in the programme is voluntary and the meetings are conducted by trained female and male volunteers from the community (see Figure 1). The adoption of positive behaviours is promoted and reinforced through repetitive, participatory activities that are designed to identify and address the barriers to, and the drivers of, behaviour change. Selected behaviours are based on their feasibility, as well as on local availability and access to materials, and include cooking demonstrations, micro-gardening, building replicable latrines, handwashing points, rubbish pits, utensil drying racks and fuel-efficient stoves as well as learning active health-seeking behaviours and food processing, preservation and storage techniques.
Figure 1. Overview of the Nutrition Impact and Positive Practice approach1
The implementation of the approach is guided by the NIPP implementation guidelines (GOAL, 2016) and toolkit which support planning, implementation, monitoring and communication. The NIPP toolkit includes separate implementation frameworks for female and male groups. For females, the framework involves the assessment of caregivers and children at enrolment (baseline), the monitoring of attendance at meetings and measuring mid-upper-arm-circumference (MUAC) across the 12-week series of meetings. Upon graduation, the initial assessment is repeated and the participants are classified as successful, defaulted, non-response or referred. To assess maintenance of knowledge and practices, a randomly selected sub-sample of graduated children and pregnant and lactating women (PLW) (N=82 per intervention area) are followed up at two months, six months and 12 months post-graduation.
GS has reached over 8,561 caregivers with NIPP and approximately 42,805 household members directly benefitted from the programme between 2013 and 2019. This article presents the findings from an independent evaluation conducted by Action Against Hunger UK’s Monitoring, Evaluation and Learning Services (AAH-MS) in 2019 to (1) evaluate the effect of NIPP on moderate acute malnutrition (MAM) prevention and treatment in children 6-59 months of age; and (2) perform a cost-efficiency analysis.
Methods
This evaluation used a mixed-methods design, including both quantitative and qualitative assessments, and a cost analysis. NIPP’s longitudinal monitoring collects over 20 indicators on knowledge, behaviours and anthropometry from all participants at baseline and graduation and from a representative sample at three time points up to 12-months post-graduation. GS’s database containing 5,017 data points was used for the quantitative analysis. The data was categorised into the following areas: care practices, feeding practices, micro-gardening and livelihood practises plus hygiene and sanitation practices. A group of variables was selected for each practice area and built into regression models to estimate NIPP’s effect on MAM treatment and to identify the behavioural predictors of improved nutrition status from baseline to graduation.
The same categorisation of practice areas and variables was used to analyse MAM prevention. This analysis assessed the degree to which the NIPP approach has a long-lasting impact on behaviour change and MAM status. Due to data limitations, descriptive analysis rather than regression models was used to analyse post-graduation follow-up data. Finally, the cost analysis used expenses data for three NIPP programme periods between May 2016 and May 2019, along with the number of NIPP groups and participants, to identify the expenses related to running the programme as well as the average cost to treat MAM.
Results
Of the 5,017 data points analysed in this evaluation, 3,808 represented children 0-59 months. Of these 3,808 children, 1,807 (47.5%) were male and 1,999 (52.5%) were female.
MAM prevalence decreased from 87% at baseline to 4% at graduation in children 6-59 months of age, corresponding to a 95% cure rate (N=3,385) (see Figure 2). Of the 167 children for whom data was collected from graduation to 12-month post-graduation, 93% experienced improved MUAC measurements (N=155) while 6% deteriorated. None were classified as malnourished during this period.
Figure 2. Distribution of mid-upper arm circumference for children under five years of age enrolled in the Nutrition Impact and Positive Practice programme at baseline and graduation.
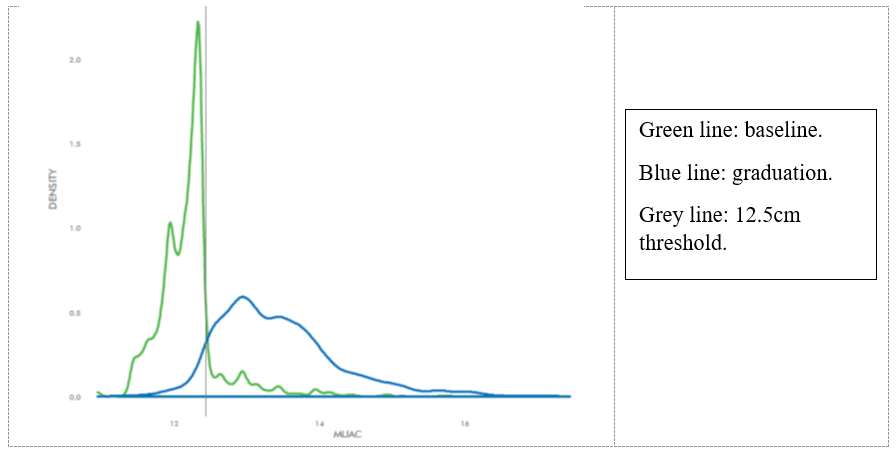
The majority of the 19 knowledge and behaviour indicators analysed improved during the 12-week cycle and were either sustained or improved at 12-months post-graduation. The most noteworthy decline in positive practices at 12 months was related to micro-gardening and this was confirmed by the qualitative analysis. For most of the indicators, an improvement from baseline to graduation was associated with an improvement in child MUAC except for two behaviours: having a latrine (non-significant) and having a micro-garden (significant). The direct expenses required to cure a child from MAM through NIPP in Sudan was estimated at €42.90.
Limitations
Of the 5,017 cases in the Sudan dataset, 445 children and PLW were sampled and followed up from graduation to two-months post-graduation. Only 201 of these cases were followed up to 12-months. This loss-to-follow-up between graduation and 12 months may have biased the post-graduation analysis. A retrospective qualitative assessment conducted by GOAL in 2015 in Malawi and Zimbabwe showed that migration for work or economic reasons was the main reason for loss-to-follow-up after NIPP graduation (unpublished). While GOAL has included migration as an exclusion criterion for enrolment to minimise attrition during the 12-week NIPP cycle, they have limited control over loss-to-follow-up after graduation.
The cost-efficiency analysis was limited to project expense data and did not include an analysis of support or societal costs which would contribute to the total cost of programme implementation. Some societal costs, i.e., financial costs incurred by the caregivers in relation to micro-garden and latrine constructions, were mentioned by participants in the qualitative assessment. However, a full cost-effectiveness analysis is needed to fully understand the societal costs and how these affect uptake and maintenance of behaviours.
Lessons learnt
NIPP was designed to holistically address the underlying behavioural drivers of malnutrition in children and mothers through multi-sector, gender-sensitive actions. However, during its early iterations, the approach focused on sector-specific technical support for individual activities. For example, livelihood specialists supported on micro-gardening, WASH specialists on handwashing, latrines and other hygiene-promoting elements, health specialists on active health-seeking behaviours and nutrition specialists on M-ICYF, care and cooking demonstrations. This fragmented approach failed to engage families in daily activities across sectors and was restricted by the need for collaboration between different sectoral leads. NIPP has since been redesigned (between 2015 and 2017) as a more integrated and inclusive approach which pulls together the multi-sector, behavioural determinants of malnutrition where the use of peer-led support, practice and repetition enables participants to simultaneously improve multiple behaviours within their daily routines. Internal and external evaluations such as this have informed this process.
The positive effects of the NIPP approach may be linked to its foundation in a theory of change (ToC) model (Harris-Fry et al, 2020). The NIPP ToC is built around three impact pathways including (1) cross-sector and practical behaviour change sessions designed to improve child feeding and care practices by increasing female and male caregivers’ knowledge and skills around M-IYCF, hygiene-sanitation and health-seeking behaviours as well as by triggering households’ construction and use of hygiene-enabling facilities; (2) participatory cooking demonstrations using locally available and accessible foods to make high-energy, nutrient dense recipes; and (3) micro-gardening and food processing, preservation and storage techniques designed to improve household year-round access to and consumption of diversified and nutritious foods. These impact pathways all contribute to an improved health and nutrition status.
It should be noted that although NIPP has the potential to address different manifestations of malnutrition (wasting, stunting or micronutrient deficiencies), anthropometric outcomes focus on wasting measured by MUAC in conjunction with behavioural and health indicators. The reason for this is attributable to (1) the operational simplicity and accuracy of the MUAC tool compared to tools used for taking weight and/or height measurements in community contexts; and (2) the relatively short timeframe of the NIPP approach where, according to a recent brief published by the United States Agency for International Development Advancing Nutrition (USAID, 2020) stunting should be used as an indicator of the overall wellbeing of a population rather than as a primary indicator of the success or failure of short-term or single nutrition interventions. This suggests that, even if feasible, linear growth may not be a relevant indicator of effectiveness for a programme such as NIPP.
This evaluation has revealed that NIPP participants in Sudan faced challenges in establishing and/or sustaining their micro-gardens after graduation. Similar findings were reported in Niger and Malawi in 2017 and 2018 respectively. In Sudan, a lack of water, particularly during the dry season, and limited access to seeds and tools were found to limit the uptake and/or maintenance of micro-gardening. While the implementation guidelines for the NIPP approach (GOAL, 2016) considers water access, the labour-intensive agricultural season and contextually appropriate agricultural practices, they have not explicitly considered the dry season or the size of micro-gardens. The evaluation has also put an emphasis on incorporating climate-resilient agricultural techniques and sustained access to climate-resilient seeds or nutritionally improved seeds to ensure the sustainability of micro-gardens. In Sudan, these factors have been addressed in the NIPP micro-gardening component through the promotion of small-scale micro-gardens, the provision of improved seeds, the inclusion of climate-smart agriculture techniques in the NIPP curriculum and by linking NIPP communities to agro-dealers through community fairs. Despite the challenges faced, it is still deemed an important component for inclusion in communities who produce much of their own food.
As mentioned, attrition during the post-graduation follow-up has restricted analyses at this time point. GOAL therefore collaborated with an independent biostatistician in the last quarter of 2021 to revise the NIPP sampling framework. The updated framework incorporates a larger sample size for follow-up, but with a reduced timeframe, whereby longitudinal data will only be collected until six-months post-graduation. Having a larger, representative sample will allow for more complex analyses that will contribute to the further development of MAM prevention programmes.
Conclusion and next steps
Findings from the AAH-MS evaluation of NIPP in Sudan are similar to the findings from the analysis of GOAL’s global NIPP dataset including data for 12,570 children collected over five years of implementation across five sub-Saharan countries (unpublished analysis). These findings highlight the contribution of NIPP to reducing MAM in children under five years of age as well as to improved nutrition, hygiene and health-seeking behaviours. The direct cost per child for MAM treatment through NIPP in Sudan was estimated at €42.90 (~$48.07). A 2019 study conducted in Mali reported average costs of $89.01 and $90.43 per child for MAM treatment using ready-to-use supplementary food or corn–soy blend++ respectively (Isanaka, 2019). Although these costs are not directly comparable due to contextual differences and the absence of standardised methods for cost analysis, this highlights the potential cost-efficiency of community-based interventions for undernutrition like NIPP. Sustainability and the duration of impact are also key considerations when comparing interventions since the impact of food-based, input driven interventions such as those evaluated in Mali is often limited to the implementation period, unlike NIPP.
It is important that donors, practitioners and governments acknowledge the need for long-term funding to progress research and programming efforts to address undernutrition. The findings from this evaluation contribute to the evidence base on community-based social behaviour change communication strategies for the prevention and treatment of undernutrition and can be used to advocate for increased buy-in and funding for NIPP scale-up in Sudan and beyond. Building on the positive achievements of NIPP, GOAL worked with the Sudan Federal Ministry of Health (FMoH) in 2018 to set up a national NIPP Technical and Advisory Service (NTAS) supporting NIPP scale. NTAS has led NIPP institutionalisation in Sudan with the FMoH formally endorsing the NIPP implementation guidelines in April 2021. Together with this technical hub, GOAL will continue to support NIPP implementation in Sudan while progressing the research agenda on the prevention of malnutrition.
For more information, contact Marlene Hebie at: mhebie@goal.ie
References
de Onis M, Borghi E, Arimond M, Webb P, Croft T, Saha K et al (2018) Prevalence thresholds for wasting, overweight and stunting in children under 5 years. Public Health Nutrition 22(1): 175–179. https://10.1017/S1368980018002434
Development Initiatives (2018) 2018 Global Nutrition Report: Shining a light to spur action on nutrition. Bristol, UK: Development Initiatives.
GOAL (2016) Implementation guidelines for Nutrition Impact and Positive Practice (NIPP) approach. GOAL Ireland - October 2016. https://resources.acutemalnutrition.org/NIPP-Implementation-Guidelines_2016.pdf
Harris-Fry H, O'Hearn M, Pradhan R, Krishnan S, Nair N, Rath S et al (2020) How to design a complex behaviour change intervention: experiences from a nutrition-sensitive agriculture trial in rural India. BMJ Global Health 5: e002384. https://doi.org/10.1136/bmjgh-2020-002384
Isanaka S, Barnhart, DA, McDonald CM et al (2019) Cost-effectiveness of community-based screening and treatment of moderate acute malnutrition in Mali. BMJ global health, 4(2), e001227. https://doi.org/10.1136/bmjgh-2018-001227
UNICEF (2019) The State of the World’s Children 2019. Children, food and nutrition: Growing well in a changing world. UNICEF, New York.
USAID Advancing Nutrition. 2020. Stunting: considerations for use as an indicator in nutrition projects. Arlington, VA: USAID Advancing Nutrition.
1 Definition of abbreviations in diagram: LLH refers to Livelihoods; CI refers to Chronically Ill


