Human milk: A win-win-win for health, sustainability, and economics?
Julie Smith Honorary Associate Professor and ARC Future Fellow at The Australian National University
Alessandro Iellamo Independent Consultant
Tuan Nguyen Technical Advisor at Alive & Thrive East Asia Pacific, FHI 360 Global Nutrition
Bindi Borg Independent consultant
Roger Mathisen Director of Alive & Thrive East Asia Pacific and the Global Nutrition Innovation Incubator at FHI 360
Thomas Stubbs Field Exchange Coordinator at Emergency Nutrition Network (ENN)
The full research and development teams for the Mothers’ Milk Tool1 and the Green Feeding Tool2 are listed below.
What we know: Breastfeeding is important for health, but until now its broader environmental and economic significance has been in the shadows.
What this adds: Two new resources – the Mothers’ Milk Tool and the Green Feeding Tool (Smith et al., 2023a; 2023b) – switch on the light by calculating the environmental costs and economic losses of not breastfeeding. Launched by the Australian National University and Alive & Thrive, with the support of the FHI 360 Global Nutrition Innovation Incubator, these tools are an important step forward in filling vast data gaps. This article explores how, by enabling breastfeeding, we contribute not only to health but also to environmental and economic goals, making this an investable solution for multiple sectors.
An evolved ‘health food’
As well as being foundational for good nutrition and health, breastfeeding has broader importance. Breastfeeding’s nutritional, immunological, developmental, emotional, and – as we articulate here – economic and environmental significance cannot be overstated amidst the sustainable development challenges of the 21st century.
Breastfeeding is so uniquely adaptable to changing disease environments that it is commonly referred to as ‘the first vaccination’. Amidst emergencies or disasters and rising food insecurity, breastfeeding provides immediate and safe nutrition and care for infants and young children.
The nutrient balance of breastmilk is ‘precision engineered’ via evolutionary processes for optimum child growth and development. The publicity around artificial intelligence is a relevant reminder that breastfeeding women provide a dynamic fluid capable of its own form of ‘machine learning’. Infant saliva transfers chemicals to a mother’s body that adjusts milk composition based on the evolving needs of the child – just one of the many complex ways that breastfeeding and human milk adapt to nourish the child.
The protection goes beyond the infant. Breastfeeding also reduces women’s reproductive cancers and type 2 diabetes, as well as a host of non-communicable diseases. Breastfeeding also helps child spacing through its hormonal effects. In the age of biohacking, 3D-printed drugs, and personalised nutrition, it is ironic that a natural, essential, and universal practice of the past provides such a tailored and personalised health solution in today’s world. It is, in short, a uniquely potent, broad-spectrum ‘health food system’.
With adequate societal and familial support, most women can breastfeed. When a biological mother cannot breastfeed, wet nursing, milk sharing, and donor milk from human milk banks can be acceptable alternatives. However, the food industry has succeeded in marketing manufactured substitutes – commercial milk formula (CMF) – as a globally acceptable “next best” product.
Despite its unique superiority, fewer than half of infants aged 0–6 months are exclusively breastfed globally. Regionally, South Asia has the highest prevalence (61%), yet just one in three infants are exclusively breastfed in the Middle East and North Africa. We must do more to restore breastfeeding as a universal practice.
Where health arguments might not gain traction, can we advocate for breastfeeding through an additional lens?
Sustainability
The global food system accounts for a third of greenhouse gas emissions, and CMF is among the high emission foods at the centre of the problem – meat and dairy.
CMF products, including infant and follow-on formula milk, are predominantly dairy based. The dairy industry requires vast amounts of land and produces a significant amount of greenhouse gas emissions. Each kilogram of CMF produced is responsible for generating between 11 and 14kg of carbon dioxide (equivalent) greenhouse gas over the full product life cycle, including emissions from milk production and powder manufacture, transport, and feeding equipment and sterilisation. A kilogram of CMF requires well over 5,000 litres of water, with associated water pollution, and waste from packaging and feeding bottles also harms the environment.
“Feeding an infant fully for six months with CMF instead of breastfeeding is estimated to generate between 226 and 288kg of CO2”.
CMF was introduced decades ago to improve nutrition for infants that were not breastfed. Now, with billions of dollars used globally to increase demand and sales, in 2020 CMF products generated around US$55 billion annually in sales; at least US$2.6–3.5 billion is invested by industry to market these products to a wide population (Baker et al., 2023). Since health facility and household use of CMF is far beyond medical necessity, might we reduce its contribution to our increasingly unbalanced carbon equation?
There are two routes to mitigating the environmental impacts of products with high carbon footprints: decarbonising production processes or reducing demand/consumption. For CMF, we highlight research (Long et al., 2021) showing that reducing consumption would far exceed the greenhouse gas emission reduction from decarbonising the production process of CMF products while simultaneously improving the health of infants, mothers, and nations. In fact, rather than reducing emissions at all, decarbonisation may assist CMF marketing by ‘greenwashing’ these products, which would instead work to increase overall CMF emissions.
“The high prevalence of CMF use generates significant greenhouse gas and environmental impacts. By contrast, breastfeeding substantially mitigates emissions...”
Regarding the decarbonisation route, the United Nations Clean Development Mechanism (CDM) is currently the largest carbon offset scheme arising from the 2015 Paris Agreement. It allows countries to fund greenhouse gas emissions-reducing projects in other countries and claim the saved emissions as part of their own efforts to meet their agreed emissions-reduction targets. CDM projects must fulfil specific criteria to receive funding and are required to demonstrate greenhouse gas emission reductions while contributing to sustainable development as defined by the host country.
However, measures promoting low-carbon diets that reduce the consumption of meat and dairy are not currently considered under the CDM. Nor are interventions that reduce CMF production and consumption. Strong evidence exists for the feasibility and effectiveness of key interventions to protect, support, and promote breastfeeding.
Adjusting CDM funding criteria to include these key breastfeeding interventions is an important action that would support countries to implement such measures, as well as going some way toward addressing gender equality issues.
To provide a basis for developing a new CDM methodology to include interventions aimed at increasing exclusive breastfeeding and reducing CMF feeding in carbon-offset calculations, Smith et al. (2023a) developed a ‘Green Feeding Tool’. This digital tool calculates both the carbon and water footprints of CMF at country and global levels. The estimation is based on available data on feeding practices of children under six months of age, as well as studies of the greenhouse gas emission and water use impacts of CMF.
As a next step, the Green Feeding Tool team will advocate for the tool’s incorporation into existing carbon offset schemes and footprint calculators. As well as providing a resource to support governments and other stakeholders to mitigate climate impacts, the tool can support progress toward the World Health Assembly’s Global Nutrition Targets for breastfeeding. The Green Feeding Tool complements the Mothers’ Milk Tool described below.
The economy
There are three main aspects to the economic value of breastfeeding:
First, a ‘micro’ approach to valuing it is to quantify the financial and human costs of higher rates of stunting, wasting, cognitive losses, and infectious disease and non-communicable diseases that result from insufficient breastfeeding. The Cost of Not Breastfeeding Tool assesses these costs in monetary and mortality terms (Walters et al., 2019).
Second, there is the ‘macroeconomic’ value of breastfeeding – productivity in the form of the uniquely valuable food and nutrition for infants and young children provided by breastfeeding women or, against this, the ‘lost milk’ in countries with low breastfeeding rates.
Third, there are the ‘investments’ – maternal and societal – needed for breastfeeding. Women and families invest time, energy, and skills so that children are breastfed (Smith and Forrester, 2013). Societal investments include, for example, adequate paid maternity leave, which demonstrably improves breastfeeding rates and the health of both mother and child. Investments to counter the influence of CMF industry marketing and reform maternity care practices are also needed (Sanghvi et al., 2022). The World Breastfeeding Trends Initiative Costing Tool estimates the cost of investing in such measures at project, programme, or country levels (Holla-Bhar et al., 2015).
Existing tools address the first and third of these aspects, and the Mothers’ Milk Tool (Smith et al., 2023b) fills a gap on the macroeconomic aspect. The tool shines a light on the economic value contributed to society by women's unpaid care work through breastfeeding infants and young children. The tool is built on 50 years of research and a breakdown of the methods employed can be found in the original paper.
The Mothers’ Milk Tool shows the substantial quantities of human milk produced by breastfeeding mothers and provides estimates of its monetary value to countries. It also shows the value that can be lost if mothers are taken for granted or left unsupported in their efforts on breastfeeding. The authors reiterate that current national accounting practices – specifically, the measurement of gross domestic product (GDP) – count CMF production in GDP but do not count human milk production.
But why does this matter? Well, by not assigning a monetary value to something, it is seen as “worthless” in economic terms. This makes it harder to advocate for and assign appropriate policies and investments to enable women to breastfeed without hardship. To illustrate the importance of this mismeasurement of economic “value”, Nobel prize-winners Amartya Sen and Joseph Stiglitz observe that human milk needs to be included in conventional GDP for policymakers to have less biased visibility of what is valuable.
By providing macroeconomic estimates for around 140 countries, the Mothers’ Milk Tool highlights that considering women’s breastfeeding capabilities in economic terms is both justifiable and feasible. It also fills a gap in the calculations of GDP. For individual mothers, it provides calculations highlighting the importance of the unpaid care work of breastfeeding infants and young children.
“The Mothers’ Milk Tool uses a price of USD 100 per litre to place a monetary value on the amount of human milk produced by breastfeeding women each year.”
An important element of the tool is its estimates of how much breastmilk the world’s women produce each year. This underpins calculations of the monetary value. The unit price of human milk that the tool applies to calculate this value is very conservative. It uses the price of fresh human milk exchanged within a not-for-profit milk bank network in Norway’s public health system – about USD 100 a litre. This may not extrapolate to other country settings. For example, a cost analysis from Italy estimated the average cost of supplying pasteurised donor milk to be USD 245 per litre (roughly USD 7 per ounce).
The exchange price in Norway reflects a not-for-profit rather than a market-based value. Its milk banks mostly use screened but unpasteurised milk, which is what the Mothers’ Milk Tool is measuring at country level. Norwegian society places a high value on breastfeeding and breastmilk in regard to child development and health services. Only Norway counts mothers’ milk in its food supply (Smith et al., 2022), and the Mothers’ Milk Tool uses a similar algorithm.
The tool estimates that the world loses USD 2.2 trillion in value every year (almost 10% of US GDP and 12% of China’s GDP in 2022) to a lack of breastfeeding. This is because 38.2% of breastmilk is currently ‘lost’ (Table 1). Lost milk provides an indicator of the vulnerability and potential food insecurity of children in emergencies.
Users of the tool have endorsed it for training health professionals and building mothers’ confidence about the importance of their efforts. The tool has also been endorsed as a tool for advocacy to policymakers for greater investment in breastfeeding protection, promotion, and support. National accountants also see it as useful to informing policymakers about the non-monetary productive sector of the economy. Mothers have been inspired and boosted by it, with testimonials available on YouTube.3
Table 1: Estimated amount of actual and potential human milk production by country for children aged 0–36 months
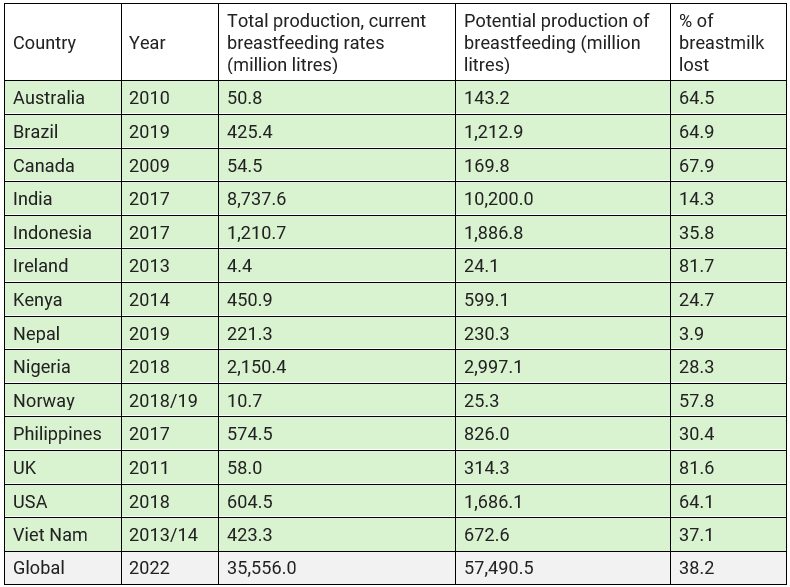
Breastmilk lost is the total production compared to amounts if 98% of children born each year were breastfed in line with WHO infant and young child feeding recommendations.
Conclusion
Both tools can be used to strengthen advocacy for policies and programmes supporting mothers to meet their individual breastfeeding goals, as well as cost savings to health systems and society from doing so. Such policies include more supportive maternity care practices, adequate maternity leave, and more supportive work environments, as well as more rigorous laws or regulations preventing exploitative marketing of CMF to health professionals and the public. These tools also highlight the need for adequate data to monitor and measure how infants and young children are being fed as the basis for suitable policies and programmes to be put in place where needed.
For more information, please contact Julie Smith at julie.smith@anu.edu.au
References
Baker P, Smith J, Garde A et al. (2023) The political economy of infant and young child feeding: Confronting corporate power, overcoming structural barriers, and accelerating progress. The Lancet, 401, 10375, 503–524.
Holla-Bhar R, Iellamo A, Gupta A et al. (2015) Investing in breastfeeding – the world breastfeeding costing initiative. International Breastfeeding Journal, 10, 8.
International Labour Organization (2022) Care at work: Investing in care leave and services for a more gender equal world of work. ilo.org.
Long A, Mintz-Woo K, Daly H et al. (2021) Infant feeding and the energy transition: A comparison between decarbonising breastmilk substitutes with renewable gas and achieving the global nutrition target for breastfeeding. Journal of Cleaner Production, 324.
Sanghvi T, Homan R, Forissier T et al. (2022) The Financial Costs of Mass Media Interventions Used for Improving Breastfeeding Practices in Bangladesh, Burkina Faso, Nigeria, and Vietnam. International Journal of Environmental Research and Public Health, 19, 24.
Siregar A, Pitriyan P, Walters D et al. (2019) The financing need for expanded maternity protection in Indonesia. International Breastfeeding Journal, 14, 27.
Smith J & Forrester R (2013) Who Pays for the Health Benefits of Exclusive Breastfeeding? An Analysis of Maternal Time Costs. Journal of Human Lactation, 29, 547–55.
Smith J, Borg B, Iellamo A et al. (2023a) Innovative financing for a gender-equitable first-food system to mitigate greenhouse gas impacts of commercial milk formula: Investing in breastfeeding as a carbon offset. Frontiers in Sustainable Food Systems, 7.
Smith J, Iellamo A, Nguyen T et al. (2023b) The volume and monetary value of human milk produced by the world’s breastfeeding mothers: Results from a new tool. Frontiers in Public Health, 11.
Smith J, Lande B, Johansson L et al. (2022) The contribution of breastfeeding to a healthy, secure and sustainable food system for infants and young children: Monitoring mothers’ milk production in the food surveillance system of Norway. Public Health Nutrition, 25,10, 2693–2701.
Walters D, Phan L & Mathisen R (2019) The cost of not breastfeeding: Global results from a new tool. Health Policy and Planning, 34,6, 407–417.
About This Article
Jump to section
Download & Citation
Reference this page
Julie Smith, Alessandro Lellamo, Tuan Nguyen, Bindi Borg, Roger Mathisen, Thomas Stubbs (2024). Human milk: A win-win-win for health, sustainability, and economics? Field Exchange Magazine 72. https://doi.org/10.6084/m9.figshare.25443652


